- Varicose veins and spider veins are very common.
- Visible veins are not only a cosmetic problem.
- Varicose and spider veins are a sign of underlying disease.
- Genetics, age, and lifestyle factors can influence the development of varicose and spider veins.
- Vein disease can place you at risk for serious health issues.
- Deep Vein Thrombosis (DVT)
- Pulmonary Embolism
- Venous Ulcers
- Vein treatment is available.
If you have varicose veins or spider veins, or are at risk for developing them, you may be interested in learning more about your overall vein health.
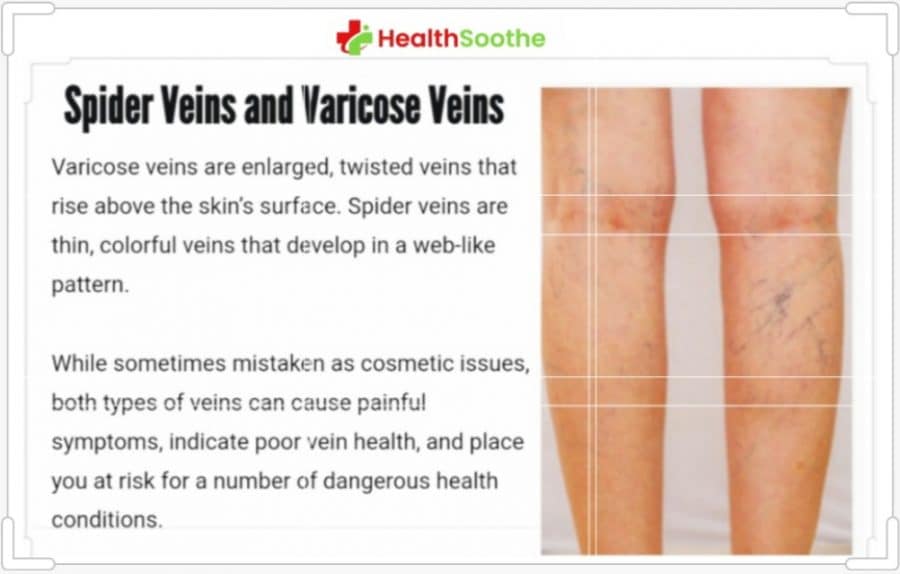
Varicose veins are enlarged, twisted veins that rise above the skin’s surface. Spider veins are thin, colorful veins that develop in a web-like pattern.
While sometimes mistaken as cosmetic issues, both types of veins can cause painful symptoms, indicate poor vein health, and place you at risk for a number of dangerous health conditions.
Below, we cover six essential things that you should know about spider veins and varicose veins. To learn more, we recommend consulting a vein specialist.
Varicose veins and spider veins are very common.
If you suffer from venous issues, you are far from alone. In fact, you may be surprised to learn just how common varicose and spider veins are.
In the United States, approximately 23% of adults have varicose veins. Since they are more common in women than men, this equates to 22 million women and 11 million men between the ages of 40 to 80 years.
When spider veins and reticular veins are also considered, the prevalence increases to 80% of men and 85% of women. Reticular veins are a third type of malfunctioning vein; they are larger than spider veins, though smaller than varicose veins.
Visible veins are not only a cosmetic problem.
Let’s face it: varicose veins and spider veins can be unsightly. However, they can also cause a range of painful and uncomfortable symptoms, impacting your quality of life. Most commonly, the legs, ankles, and feet are affected.
Varicose vein symptoms can include:
- Heavy legs
- Swelling
- Numbness
- Itching and Burning
- Pain Relief When Legs are Elevated
Although spider veins are less likely than varicose veins to cause pain and discomfort, potential symptoms can include:
- Swelling
- Leg restlessness, especially at night
- Tingling, numbness, burning, or itching
- Tenderness or redness surrounding impacted veins
If you experience any of the above issues, we want you to know that help is available. Early treatment can alleviate symptoms and prevent them from becoming worse.
Varicose and spider veins are a sign of underlying disease.
Your veins play a critical role in your body’s circulatory system. While the arteries transport oxygenated blood to your legs and throughout the body, your veins are responsible for transporting oxygen-depleted blood back to the heart for reoxygenation.
Varicose veins and spider veins are caused by underlying vein disease, also known as venous insufficiency. Vein disease is a progressive condition, meaning that symptoms get worse over time. Vein disease develops when veins are placed under chronic strain due to a range of factors, including genetics, age, and lifestyle. Over time, strained veins can lead to the malfunctioning of tiny, one-way vein valves in the legs.
When vein valves begin to malfunction, they are unable to transport enough blood against gravity back to the heart. As a result, blood pools or flows backward in the lower extremities. Also known as “leaky” veins or venous reflux, this condition is what leads to the development of varicose veins and spider veins.
Genetics, age, and lifestyle factors can influence the development of varicose and spider veins.
Although you may be wondering how to prevent or manage vein disease, the reality is that some risk factors are out of your control.
These include:
- Genetics: If you have a parent with varicose veins, you are more likely to develop them. If both parents are affected, your risk further increases.
- Age: Although anyone can develop vein disease, individuals over age 40 are more susceptible.
- Sex: Women are twice as likely to develop varicose veins. In part, this may be because pregnancy is also a risk factor.
To help prevent venous issues, we generally recommend you:
- Maintain a healthy Body Mass Index (BMI)
- Exercise regularly
- Eat a well-rounded diet
- Quit smoking
- Manage underlying health conditions
- Avoid prolonged standing or sitting
- Wear compression socks
- Attend routine health screenings
- Consult a vein specialist
Although following a healthy lifestyle can be beneficial, It is important to understand that this may not be enough to avoid varicose and spider veins.
Vein disease can place you at risk for serious health issues.
Along with causing varicose and spider veins, vein disease can place you at risk for a number of dangerous health conditions. These include deep vein thrombosis (DVT), pulmonary embolism, and venous ulcers.
Deep Vein Thrombosis (DVT)
Deep vein thrombosis is a type of serious blood clot that forms in the deep venous system. DVT requires immediate evaluation and treatment, since it can lead to a medical emergency known as pulmonary embolism.
DVT symptoms include:
- Swelling in the leg
- A feeling of warmth in the affected area
- Skin redness
- Pain or tenderness in your lower body, such as a cramp
Pulmonary Embolism
Pulmonary embolism is a life-threatening medical emergency that occurs when a blood clot breaks off and travels to the lungs.
Signs of a pulmonary embolism include:
- Rapid heart rate
- Difficulty breathing
- Coughing up blood
- Feeling lightheaded or faint
- Chest pain or discomfort that worsens with a deep breath or cough
If you experience any of the above, call 911 or head directly to the nearest emergency room.
Venous Ulcers
Venous ulcers are open, non-healing wounds that can form near varicose and spider veins. Although they are often mistaken for skin issues, they are actually a sign of progressing vein disease.
Venous ulcers are considered a serious issue, since they can lead to infection. If you notice skin changes near visible veins, contact your doctor as soon as possible.
Vein treatment is available.
If you suffer from symptoms of vein disease, you may be relieved to discover that you have options. These days, vein surgery is rarely necessary; instead, a range of minimally invasive, outpatient treatments, such as Ultrasound-Guided Sclerotherapy and laser procedures, can alleviate pain and discomfort.
For personalized recommendations on prevention and treatment, we encourage you to talk to your doctor or consult a vein specialist.