Nutritional information in the media around diabetes meal planning is complicated and constantly changing. Type "diabetic diet" into a search engine and you're going to get thousands of confusing results.
Should you be vegan? Low-carb? Keto? Should you cut out fat or eat nothing but fat? Everyone seems to be suggesting something different. So, what is the American Diabetes Association diet? What is the ADA diet all about?
The quick answer is there isn’t one. At least not one exact diet that will meet the nutrition needs of everyone living with diabetes. Which, in some ways, is unfortunate. Just think how simple it would be to plan meals if there were a one-size-fits-all plan that worked for everyone living with diabetes, prediabetes, or at risk for diabetes. Boring, yes, but simple!
As we all know, it’s much more challenging than that. We don’t often make food choices based on nutritional science alone —we often also make food choices for social, cultural, or emotional reasons. And because each of us is different, we each need to find an eating plan that best matches both our nutrition and lifestyle needs.
For people living with diabetes and trying to learn more about healthy food choices, it can be tough to tell facts from fiction and make decisions in a sea of choices. Information in the news can often be confusing, with conflicting data and advice often given at the same time.
Part of the job of the American Diabetes Association is to help sort out the science and provide guidance that is safe and works well for people at risk for and living with diabetes.
And current research shows there are many eating patterns that can work to maintain a healthy life with diabetes, not just one. In the long run, an eating plan that you can follow and sustain and that meets your own diabetes goals will be the best one for you.
- What Does Science Have to Say?
- What is the American Diabetes Association (ADA) Diet?
- Knowing the Best Meal Plan for You
- ADA Diet General Dietary Goals for People with Diabetes
- Knowing the Best Eating Pattern for You
- Top Eating Patterns for Diabetic Patients
- Are you Diabetic and are Looking for a Quick Place to Start to Know the Best Nutritional Advice for You?
- What You – a Diabetic Need to Know About Nutrients
- What about Glycemic Index
- The Key Takeaways
What Does Science Have to Say?
"What can I eat?" is one of the top questions asked by people with diabetes when they are diagnosed—and our goal is to help answer that question.
A panel of scientists, doctors, endocrinologists, diabetes educators, and dietitians reviewed over 600 research articles over the course of five years to see what diets—or eating patterns—work well for people with diabetes. The results were published in our Nutrition Consensus Report.
The main finding? Everyone's body responds differently to different types of foods and diets, so there is no single "magic" diet for diabetes. But you can follow a few simple guidelines to find out what works for you to help manage your blood sugar.
What is the American Diabetes Association (ADA) Diet?

There isn't such a thing as the American Diabetes Association (ADA) diet, based on the American Diabetes Association website. In other words, no one diet or food plan works for everyone who has diabetes.
Instead, the American Diabetic Association advocates for a healthy diabetes diet. A diabetic meal plan is a blueprint explaining what amount and types of food you may consume at meals and snacks.
A healthy meal plan should be compatible with your lifestyle and eating habits. The main thing is to stick to a meal plan that is personalized to personal tastes and lifestyle and assists in meeting blood glucose, blood pressure, cholesterol/triglyceride levels, and weight management objectives.
According to research, both the quantity and type of carbohydrates in a diet impact blood glucose levels.1https://healthjade.net/what-is-the-american-diabetes-association-ada-diet/ According to research, the total quantity of carbohydrates in a diet is a more reliable measure of blood glucose reaction than the Glycemic Index (GI).
According to the study, carbohydrate counting is the first strategy most patients with diabetes use to manage their blood glucose. Because carbohydrate type may alter blood glucose levels, employing the Glycemic Index could aid in "fine-tuning" blood glucose control.
In other words, when paired with carb counting, it may give an additional advantage for persons who wish and are able to put more effort towards monitoring their meal choices in order to achieve blood glucose objectives.
People with diabetes may eat the same foods as their families, but they must take additional precautions to ensure that their diet is coordinated with oral drugs and insulin, as well as exercise, to help regulate their levels of blood sugar.
This may seem to be a lot of effort, but your clinician and/or nutritionist may assist you in developing the ideal meal plan for you. Making smart eating choices can enhance your general health and may even help you avoid issues such as cardiovascular disease and certain malignancies.
The appropriate meal plan can assist you in improving your glucose levels, blood pressure, as well as cholesterol readings while also helping you stay on track with your weight. Your food plan might help you lose weight or maintain your current weight.
Because there is no such thing as a perfect cuisine, having a variety of foods and monitoring portion sizes is essential for a balanced diet. Also, ensure that the nutrients you choose from each food category are of the greatest quality possible. In other words, choose foods high in vitamins, minerals, and fiber over-processed meals.
Everyone benefits from good eating, so the whole family may participate. You may include your favorite meals in your food plan while still managing your sugar levels, blood pressure, and cholesterol.
Foods labeled 'diabetic' or 'suitable for diabetics' should be avoided. These meals have comparable calorie and fat content and may impact your glucose levels. They are typically more costly and might cause constipation. Stick to your regular diet. If you wish to indulge on occasion, stick to your regular favorites and watch your quantities.
There is no such thing as a "diabetic diet." A healthy diet helps maintain your blood sugar levels within the normal range. Controlling your blood glucose levels is an important element of treating your diabetes since it may avoid diabetic complications.
Healthsoothe has an article that showcases a simple plan on how to manage your diabetes. You can read it here, and the Centers for Disease Control and Prevention offers a free recipe booklet for diabetics and their families, which may be downloaded here.
A trained dietician may also assist you in developing a personalized dietary plan. It should include your weight, medications, lifestyle, and any other health issues you may have.
To calculate your body mass index (BMI), use Healthsoothe’s powerful and accurate Free Online BMI Calculator for Adults and Children.
You may use a free, award-winning, cutting-edge online diet and exercise monitoring program called SuperTracker from the US Department of Agriculture Center for Nutrition Policy and Promotion to figure out What and How Much To Eat.
This free program enables you to create a healthy diet, control your weight, and decrease your likelihood of chronic food-related disorders. SuperTracker can help you decide how much and what to eat, monitor your meals, physical activity, and weight, and customize your experience with goal setting, online coaching, and blogging.
You may use our free online tool Body Weight Planner to figure out the number of calories you should consume to lose weight based on your weight, age, gender, height, and physical activity.
You may use the free web app ChooseMyPlate to learn about the Food Groups you ought to include in your dish for a meal.
Read also:
How to Manage Type2 Diabetes with Exercise
Look and Feel Your Best: 6 Ways to Improve Your Health
Tips for a Healthy Diet and Nutrition for Women
Knowing the Best Meal Plan for You
A meal plan takes into account your likes, dislikes, and lifestyle. It is a guide that is aimed at helping you meet your personal weight and blood glucose goals and guides you on what, when, and how much to eat.
While many people may think a meal plan is the same as a diet, we like to consider a meal plan as something you follow over time rather than a diet, which is often related to a quick fix for a short period of time.
ADA Diet General Dietary Goals for People with Diabetes
Nutrition treatment objectives for people with diabetes have developed in recent years, becoming more adaptable and user-friendly.
These objectives include the following:
To encourage and support healthy eating habits, emphasizing a range of nutrient-dense meals in appropriate portion sizes, in order to enhance general health and, more particularly, to:
Attain personalized blood pressure, lipid, and glycemic targets. The ADA's general suggested targets for these indicators are as follows:
- A1C less than 7%
- 140/80mmHg level of blood pressure
- 100 mg/dL level of LDL cholesterol
- 150 mg/dL level of triglycerides
- Men with HDL cholesterol levels of more than 40 mg/dL
- Women with HDL cholesterol levels of more than 50 mg/dL
- Reach and keep body weight targets
- Delayed or avoided diabetes problems.
- Individual dietary requirements must be addressed based on individual and varying perspectives, health knowledge and numeracy, availability of healthy food options, desire and capacity to adopt behavioral changes, and obstacles to change.
- To sustain the enjoyment of eating by sending positive signals regarding food choices while restricting food decisions only when scientific evidence suggests it.
- Rather than concentrating on specific macronutrients and micronutrients, provide the diabetic with approaches and tools for daily meal planning.
- Individual A1C, blood pressure, and cholesterol targets may need to be altered depending on age, diabetes duration, health history, and other current health issues. The ADA Standards of Medical Care in Diabetes provide further guidelines for goal individualization.
The key to eating well with diabetes is to consume a variety of healthful meals from all food categories in the proportions recommended by your meal plan. As a result, the American Diabetes Association established:
- Meal Plans for Diabetics and
- An online diet provider and checker tool called Create Your Plate (also known as Diabetes plate method): Fill your dish with more non-starchy vegetables and lower quantities of starchy foods and proteins with the Create Your Plate method—no special equipment or counting necessary. You can use this interactive tool to practice.
To know more on the American Diabetes Association diet guidelines, watch the video below:
Knowing the Best Eating Pattern for You
An eating pattern is a term used to describe the foods or groups of foods that a person chooses to eat on a daily basis over time. There are a number of eating patterns that are helpful for people living with diabetes or at risk for diabetes.
Following are a few of the more popular choices that the science shows can work. You’ll notice that all of these have three things in common:
- Plenty of non-starchy vegetables such as broccoli, green beans, kale, and salad greens
- Lean protein foods including meat, chicken, fish, shellfish, eggs, cheese, nuts, seeds, and plant-based protein foods like soy and beans are included in differing proportions
- A focus on healthy fats—including vegetable oils like olive, canola, and sunflower—and limitations on solid fats like butter, lard, and margarine.
There is no "one-size-fits-all" eating plan or "ADA Diet" for people with diabetes! The best eating plan for you is the one that you can sustain while still meeting your diabetes goals.
Top Eating Patterns for Diabetic Patients
- The Mediterranean Eating Pattern: Mediterranean-style eating uses olive oil as the main source of fat. Fish, chicken, and small amounts of dairy products, such as cheese and yogurt, are included. Red meat is less common, though wine can usually be consumed in small amounts (one to two glasses of wine per day) with meals. There is a lot of research on the Mediterranean style of eating and most of it shows it may help you improve blood sugar, lose weight, and reduce the risk of heart disease, stroke, and some cancers. This is a well-studied eating pattern that can work for many people with diabetes.
- The Vegetarian or Vegan Eating Pattern: Vegetarian eating plans generally include nuts, seeds, beans, and meat substitutes with little or no animal products, though there are many eating patterns you could label “vegetarian.” These patterns are different in terms of protein sources, from vegan eating plans that include no animal products of any kind to new patterns, such as flexitarian eating plans that include mostly plant-based foods but allow for eating meat at times.
- The Low-Carbohydrate Eating Pattern: A low-carbohydrate (low-carb) eating plan includes protein foods like meat, chicken, fish, shellfish, eggs, cheese, nuts and seeds, and fats (oils, butter, olives, and avocado). Most low-carb plans, such as Atkins, Keto, and Paleo, avoid highly processed carbohydrate foods and grains.
- The DASH Eating Pattern: DASH is an acronym for “Dietary Approaches to Stop Hypertension” and began as a research study to help lower blood pressure in people with hypertension (high blood pressure). This eating plan limits foods high in sodium (salt), saturated fat, red meat, sweets, added sugars, and sugary drinks.
You can also check:
How can I lower my Type 2 Diabetes Naturally
You can laugh at your diabetes worries if you follow this simple plan
Diabetes: Causes, Precautions, Heredity, Diagnosis, and Treatments
Are you Diabetic and are Looking for a Quick Place to Start to Know the Best Nutritional Advice for You?
Try the Diabetes Plate Method which is recommended in the American Diabetes Association Diet guidelines. Most of the eating patterns above focus on what to eat. The Diabetes Plate Method helps figure out how much to eat, which can often be just as important.2https://diabetes.org/healthy-living/recipes-nutrition
It takes the burden out of measuring and counting while meeting the goals of many of the eating patterns described above.
This method uses a 9-inch plate, often a smaller plate than most people use. Once you have a smaller plate, the idea is to fill half your plate with non-starchy vegetables, 1/4 of your plate with protein foods, and the last 1/4 of your plate with carbohydrate foods.
Using this method, you can create perfectly portioned meals with a healthy balance of vegetables, protein, and carbohydrates—without any counting, calculating, weighing, or measuring.
The Diabetes Plate Method or Create Your Plate Method
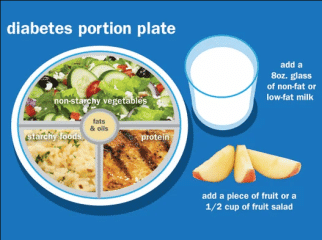
The American Diabetes Association’s Create Your Plate online interactive meal planning tool divides your daily food requirements according to the percentage daily requirement for each major food group: 25 percent Protein, 25 percent Grains, and Starchy Foods and 50 percent Non-starchy Vegetables.
Creating your plate lets you still choose the foods you want, but changes the portion sizes so you are getting larger portions of non-starchy vegetables and smaller portions of starchy foods. The healthy meal combinations are endless.
Using the 7 simple steps below to Create Your Plate you can simply and effectively manage your diabetes and lose weight at the same time. When you are ready, you can try new foods within each food category.
Try these seven steps to get started:
- Using your dinner plate, put a line down the middle of the plate. Then on one side, cut it again so you will have three sections on your plate.
- Fill the largest section with non-starchy vegetables.
- Now in one of the small sections, put grains and starchy foods.
- And then in the other small section, put your protein.
- Add a serving of fruit, a serving of dairy, or both as your meal plan allows.
- Choose healthy fats in small amounts. For cooking, use oils. For salads, some healthy additions are nuts, seeds, avocados, and vinaigrettes.
- To complete your meal, add a low-calorie drink like water, unsweetened tea, or coffee.
The food groups are:
Vegetables
A. Non-starchy Vegetables
The following is a list of common non-starchy vegetables:
- Amaranth or Chinese spinach
- Artichoke
- Artichoke hearts
- Asparagus
- Baby corn
- Bamboo shoots
- Beans (green, wax, Italian)
- Bean sprouts
- Beets
- Brussels sprouts
- Broccoli
- Cabbage (green, bok choy, Chinese)
- Carrots
- Cauliflower
- Celery
- Chayote
- Coleslaw (packaged, no dressing)
- Cucumber
- Daikon
- Eggplant
- Greens (collard, kale, mustard, turnip)
- Hearts of palm
- Jicama
- Kohlrabi
- Leeks
- Mushrooms
- Okra
- Onions
- Pea pods
- Peppers
- Radishes
- Rutabaga
- Salad greens (chicory, endive, escarole, lettuce, romaine, spinach, arugula, radicchio, watercress)
- Sprouts
- Squash (cushaw, summer, crookneck, spaghetti, zucchini)
- Sugar snap peas
- Swiss chard
- Tomato
- Turnips
- Water chestnuts
- Yard-long beans
Generally, non-starchy vegetables have about 5 grams of carbohydrates in ½ cup cooked or 1 cup raw. Most of the carbohydrate is fiber so unless you eat more than 1 cup of cooked or 2 cups of raw at a time, you may not need to count the carbohydrates from the non-starchy vegetables.
The best choices are fresh, frozen, and canned vegetables and vegetable juices without added sodium, fat, or sugar. If using canned or frozen vegetables, look for ones that say low sodium or no salt added on the label.
As a general rule, frozen or canned vegetables in sauces are higher in both fat and sodium. If using canned vegetables with sodium, drain the vegetables and rinse them with water. Then cook the rinsed vegetables in fresh water. This will cut back on how much sodium is left in the vegetables.
For good health, try to eat at least 3-5 servings of vegetables a day. This is a minimum and more is better! A serving of vegetables is:
- ½ cup of cooked vegetables or vegetable juice
- 1 cup of raw vegetable
B. Starchy Vegetables and Grains
Grains
At least half of your grains for the day should be whole grains. A whole grain is an entire grain—which includes the bran, germ, and endosperm (starchy part).
The most popular grain in the US is wheat so that will be our example. To make 100% whole wheat flour, the entire wheat grain is ground up. “Refined” flours like white and enriched wheat flour include only part of the grain – the starchy part and are not whole grain. They are missing many of the nutrients found in whole wheat flour.
Examples of whole grain wheat products include 100% whole wheat bread, pasta, tortillas, and crackers. But don’t stop there! There are many whole grains to choose from.
Finding whole-grain foods can be a challenge. Some foods only contain a small amount of whole grain but will say it contains whole grain on the front of the package. For all cereals and grains, read the ingredient list and look for the following sources of whole grains as the first ingredient:
Best Choices of Grains for Diabetics
- Bulgur (cracked wheat)
- Whole wheat flour/
- Whole oats/oatmeal
- Whole grain corn/corn meal
- Popcorn
- Brown rice
- Whole rye
- Whole grain barley
- Whole farro
- Wild rice
- Buckwheat
- Buckwheat flour
- Triticale
- Millet
- Quinoa
- Sorghum
If you suffer from Celiac disease or gluten intolerance:
- Celiac disease is a digestive disorder. When someone with celiac disease eats food containing gluten, their body reacts by damaging the small intestine. Uncomfortable symptoms such as abdominal pain often occur. The damage to the small intestine also interferes with the body’s ability to make use of the nutrients in food. About 1% of the total population has celiac disease. It is more common in people with type 1 diabetes. An estimated 10% of people with type 1 also have celiac. The only way to manage celiac disease is to completely avoid all foods that have gluten. Following a gluten-free diet will prevent permanent damage to your body and will help you feel better.
- Gluten Intolerance: There are also many people who are said to have a gluten intolerance. When these people eat foods that contain gluten, they also experience uncomfortable symptoms. However, they test negative for celiac disease and actual damage to their small intestine does not occur. More research about gluten intolerance is needed, but avoiding foods with gluten should help to relieve these symptoms.
Gluten is a protein found in wheat, rye, barley, and all foods that are made with these grains.
Starchy Vegetables
Starchy vegetables are great sources of vitamins, minerals, and fiber. The best choices do not have added fats, sugar, or sodium.
Try a variety such as:
- Parsnip
- Plantain
- Potato
- Pumpkin
- Acorn squash
- Butternut squash
- Green Peas
- Corn
Best Choices of Dried Beans, Legumes, Peas, and Lentils for Diabetics
Try to include dried beans in several meals per week. They are a great source of protein and are loaded with fiber, vitamins, and minerals such as:
- Dried beans such as black, lima, and pinto
- Lentils
- Dried peas such as black-eyed and split
- Fat-free refried beans
- Vegetarian baked beans
Fruits
Fruits are loaded with vitamins, minerals, and fiber just like vegetables. Fruit contains carbohydrates so you need to count it as part of your meal plan.3https://www.diabetesfoodhub.org/articles/ask-the-experts-what-is-the-ada-diet.html Having a piece of fresh fruit or fruit salad for dessert is a great way to satisfy your sweet tooth and get the extra nutrition you’re looking for.
The best choices of fruit for diabetics are any that are fresh, frozen, or canned without added sugars;
- Choose canned fruits in juice or light syrup
- Dried fruit and 100% fruit juice are also nutritious choices, but the portion sizes are small so they may not be as filling as other choices. Only 2 tablespoons of dried fruit like raisins or dried cherries contain 15 grams of carbohydrates so be cautious with your portion sizes!
- Includes oranges, melon, berries, apples, bananas, and grapes
For Carbohydrates Counters
- A small piece of whole fruit or about ½ cup of frozen or canned fruit has about 15 grams of carbohydrates. Servings for most fresh berries and melons are from ¾ – 1 cup.
- Fruit juice can range from 1/3 -1/2 cup for 15 grams of carbohydrates.
Fruit can be eaten in exchange for other sources of carbohydrates in your meal plans such as starches, grains, or dairy.
Proteins
The biggest difference among foods in this group is how much fat they contain, and for the vegetarian proteins, whether they have carbohydrates. Meats do not contain carbohydrates so they do not raise blood glucose levels. A balanced meal plan usually has about 2-5 ounces of meat.
Most plant-based protein foods, like beans and soy products, and any breaded meats contain carbohydrates. It’s best to read food labels carefully for these foods. In general, there are about 15 grams of carbohydrates in ½ cup of beans and between 5 to 15 grams in soy-based products like veggie burgers and “chicken” nuggets.
The best choices of protein foods for diabetics are:
- Plant-based proteins
- Fish and seafood
- Chicken and other poultry
- Cheese and eggs
Fish and Seafood
Try to include fish at least 2 times per week.
- Fish high in omega-3 fatty acids like Albacore tuna, herring, mackerel, rainbow trout, sardines, and salmon
- Other fish include catfish, cod, flounder, haddock, halibut, orange roughy, and tilapia
- Shellfish including clams, crab, imitation shellfish, lobster, scallops, shrimp, oysters.
Poultry
Choose poultry without the skin for less saturated fat and cholesterol.
- Chicken, turkey, Cornish hen
Game
- Buffalo, ostrich, rabbit, venison
- Dove, duck, goose, or pheasant (no skin)
Beef, Pork, Veal, Lamb
If you decide to have these, choose the leanest options, which are:
- Select or Choice grades of beef trimmed of fat including: chuck, rib, rump roast, round, sirloin, cubed, flank, porterhouse, T-bone steak, tenderloin
- Beef jerky
- Lamb: chop, leg, or roast
- Organ meats: heart, kidney, liver
- Veal: loin chop or roast
- Pork: Canadian bacon, center loin chop, ham, tenderloin
Cheese and Eggs
- Reduced-fat cheese
- Cottage cheese
- Egg whites and egg substitutes
Dairy
Including sources of dairy in your diet is an easy way to get calcium and high-quality protein.
The best choices of dairy products for diabetics are:
- Fat-free or low-fat (1% milk)
- Plain non-fat yogurt (regular or Greek yogurt)
- non-fat light yogurt (regular or Greek yogurt)
- unflavored fortified soy milk
If you are lactose intolerant or don’t like milk, you may want to try fortified soy milk, rice milk, or almond milk as a source of calcium and vitamin D.
Tips for Carb Counters
- 1 cup of milk or yogurt is equal to 1 small piece of fruit or 1 slice of bread
- Each 1-cup serving of milk or 6 ounces serving of yogurt has about 12 grams of carbohydrates and 8 grams of protein. Greek yogurt is higher in protein than regular yogurt, with about 12 grams per 6-ounce serving.
- If you are trying to switch to lower-fat dairy products, take the time to get used to the taste and texture difference. For example, first change from whole milk to 2%. Then to 1% or non-fat milk.
- Switching from whole to 1% milk will save you 70 calories and 4 grams of saturated fat in every serving!
Eat more fiber by eating more whole-grain foods 18. Whole grains can be found in:
- Breakfast cereals made with 100% whole grains.
- Oatmeal.
- Whole grain rice.
- Whole-wheat bread, bagels, pita bread, and tortillas.
What You – a Diabetic Need to Know About Nutrients
Now that you’ve got the basics, let’s dive into nutrients.
First things first: do you use food labels for products that you buy in the store? The food labels on packaging can be a great place to find information about the nutrients in the food you’re purchasing. You have to get smart on food labels so as to be able to determine what’s best for your body right away.
The following are the most important nutrients or food substances a diabetic person needs to control (increase or decrease) in their diet to be able to properly manage his/her diabetic condition:
Carbohydrates (Carbs):
When it comes to managing diabetes, the carbohydrates, or carbs, you eat play an important role. They impact your blood sugar, so remember that balance is key! There are three main types of carbohydrates in food—starches, sugar, and fiber.
As you’ll see on the nutrition labels for the food you buy, the term “total carbohydrate” refers to all three of these types. When it comes to choosing foods with carbs, the goal is to choose carbs that are nutrient-dense, which means they are rich in fiber, vitamins, and minerals, and low in added sugars, sodium, and unhealthy fats.
Carbohydrate items are essential in your diet. They are the finest source of energy for your body, particularly your brain. Carbohydrates are broken down in the digestive process to create glucose in circulation.
Insulin transports glucose from the bloodstream to the muscles, liver, and other cells throughout the body, where it is utilized to produce energy. Most carbohydrate-containing meals are also high in fiber, vitamins, and minerals, which help to keep our bodies and intestines healthy.
Carbohydrate is the nutrient with the greatest influence on blood glucose levels among the three essential elements in your food: fat, protein, and carbohydrate. Carbohydrate's impact is determined by:
I) the quantity of carbohydrates consumed and
II) the kind of carbohydrate consumed.
Everyone's carbohydrate requirements fluctuate based on their gender, level of activity, age, and body weight. Anyone with diabetes should consult an accredited practicing dietitian to determine how much carbohydrate to consume at each meal and snack.
All carbohydrates are digested to create glucose, but at varied rates - some slowly, others quickly. The glycemic index (GI) describes how rapidly a carbohydrate diet is processed and absorbed into the bloodstream.
Carbohydrates with a low GI enter the bloodstream slowly and have a lower influence on blood sugar levels. Lentils, thick wholegrain bread, traditional rolled oats and legumes, pasta, milk, sweet potato, yogurt, and most forms of fresh fruit are also low-GI meals.
The kind of carbohydrate you consume is important since some might induce elevated blood glucose levels after eating. Consuming modest quantities of high-fiber, low-GI carbs is the optimum combo.
A reduced carbohydrate diet could assist some individuals to control their diabetes. Consult your healthcare team for personalized guidance if you want to reduce the carbohydrate level of your diet.
Protein:
The body requires protein foods for repair and growth. Protein does not degrade into glucose, so it has no effect on blood glucose levels.
The most important protein foods are:
- Meats, poultry, fish, and tofu
- Eggs
- Nuts and seeds
- Cheese
Some protein foods with carbohydrate content, like milk, yogurt, lentils, and legumes, will affect blood glucose levels, but they should nevertheless be added as part of a balanced diet.
Calcium:
Calcium is a very important diet and it is connected to aging, diabetes, hypoglycemia, and falls. Calcium is the most abundant mineral in your body and makes up a lot of your bones and teeth.
It keeps your bones and teeth strong and supports your body’s overall structure. Calcium is also used to help your muscles move, helps with blood circulation, and your nerves to transmit messages throughout your body.
The other nutrient to know when thinking about calcium is vitamin D. Vitamin D is used to absorb calcium, so without it, it can lead to not getting sufficient amounts of calcium. Also, as we get older, our bodies aren’t as efficient in absorbing calcium.
Sugar:
Sugar can be included in a diabetes-friendly diet. It is acceptable to put a sprinkle of sugar on your porridge or a spoonful of jam on certain low GI high fiber bread. Foods laden with added sugars and low in other nutrients, on the other hand, should be consumed in moderation.
Limit high-energy foods, such as sweets, lollipops, and standard soft drinks. Several sugar can also be used in cooking, and also many recipes can be altered to use a lesser amount specified or substituted with another sweetener.
Choose recipe ideas that are low in fat (especially saturated fat) and high in fiber.
Sweeteners other than Sugar:
As previously stated, small quantities of sugar consumed as part of a well-balanced diet should not have a significant impact on glucose levels. Sweeteners like Equal, Stevia, Sugarine, and Splenda, on the other hand, may be used instead of sugar, especially if a large amount of sugar is being replaced.
Foods and drinks sweetened with a substitute sweetener, like cordials and diet soft drinks, sugar-free lollies, and so on, are also best enjoyed in moderation because they provide no nutritional benefit and frequently replace more nutritious drinks and foods such as fruits, vegetables, dairy, nuts, and water.
Water:
Water is required for the majority of bodily functions, and the body must be kept hydrated on a daily basis. Water is the best beverage to consume because it includes no additional kilojoules and has no effect on blood glucose levels.
Other viable options include:
- Water, herbal tea, tea, coffee, soda water, and plain mineral water are all options.
- If you enjoy a sweet drink on occasion, look for products labeled "diet" or "low joule."
- If you decide to drink alcohol, restrict your consumption to no more than two standard drinks per day, with alcohol-free days at least once a week.
To manage diabetes successfully, you must first fully comprehend how meals and nutrition influence your body. Portions of food and food selection are critical. To keep blood sugar levels as stable as possible, carbohydrates, fat, and protein must be balanced. (This is especially critical for individuals who have Type 1 diabetes.)
What about Glycemic Index
The glycemic index, or GI, measures how carbohydrate-containing food raises blood glucose. Foods are ranked based on how they compare to a reference food — either glucose or white bread.
A food with a high GI raises blood glucose more than a food with a medium or low GI. Meal planning with the GI involves choosing foods that have a low or medium GI. If eating a food with a high GI, you can combine it with low GI foods to help balance the meal.
Examples of carbohydrate-containing foods with a low GI include dried beans and legumes (like kidney beans and lentils), all non-starchy vegetables, some starchy vegetables like sweet potatoes, most fruit, and much whole grain bread and cereals (like barley, whole wheat bread, rye bread, and all-bran cereal).
Meat and fats don’t have a GI because they do not contain carbohydrates.
Low GI Foods (55 or less)
- 100% stone-ground whole wheat or pumpernickel bread
- Oatmeal (rolled or steel-cut), oat bran, muesli
- Pasta, converted rice, barley, bulgar
- Sweet potato, corn, yam, lima/butter beans, peas, legumes, and lentils
- Most fruits, non-starchy vegetables, and carrots
Medium GI (56-69)
- Whole wheat, rye, and pita bread
- Quick oats
- Brown, wild or basmati rice, couscous
High GI (70 or more)
- White bread or bagel
- Corn flakes, puffed rice, bran flakes, instant oatmeal
- Short grain white rice, rice pasta, macaroni, and cheese from a mix
- Russet potato, pumpkin
- Pretzels, rice cakes, popcorn, saltine crackers
- Melons and pineapple
What Affects the GI of a Food?
Fat and fiber tend to lower the GI of food. As a general rule, the more cooked or processed a food, the higher the GI; however, this is not always true.
Below are a few specific examples of other factors that can affect the GI of a food:
- Ripeness and storage time — the riper a fruit or vegetable is, the higher the GI.
- Processing — juice has a higher GI than whole fruit; mashed potato has a higher GI than whole baked potato, stone-ground whole-wheat bread has a lower GI than whole wheat bread.
- Cooking methods — how long a food is cooked (al dente pasta has a lower GI than soft-cooked pasta), frying, boiling, and baking.
- Fiber — whole grains and high-fiber foods act as a physical barrier that slows down the absorption of carbohydrates. This is not the same as ‘wholemeal’, where, even though the whole of the grain is included, it has been ground up instead of left whole. For example, some mixed-grain bread that includes whole grains has a lower GI than wholemeal or white bread.
- Fat lowers the GI of a food — For example, chocolate has a medium GI because of its fat content, and crisps will actually have a lower GI than potatoes cooked without fat.
- Protein lowers the GI of food — Milk and other dairy products have a low GI because they are high in protein and contain fat.
- Variety—converted long-grain white rice has a lower GI than brown rice but short-grain white rice has a higher GI than brown rice.
Your food choices matter a lot when you’ve got diabetes. Some are better than others. Nothing is completely off-limits. Even items that you might think of as “the worst” could be occasional treats — in tiny amounts. But they won’t help you nutrition-wise, and it’s easiest to manage your diabetes if you mainly stick to the “best” options.
The Key Takeaways
Eating right doesn’t have to be boring. When it comes to nutrition and diabetes, it’s all about finding the right balance that works for you. When you’re managing diabetes and prediabetes, your eating plan is a powerful tool.
Try to block out the fad-diet advice and choose a plan you are likely to follow long-term that fits both your diabetes goals and your personal needs. Think about your likes and dislikes and how a change to your eating will affect your day-to-day life with family and friends.
Then see how you can match this with your personal weight-loss goals. The budget also plays a part in choosing the right healthy eating plan that will meet your needs. Many eating patterns can help you maintain a healthy life with diabetes.
Food often takes center stage when it comes to diabetes. But don’t forget that the beverages you drink can also have an effect on your weight and blood glucose!
The ADA Diet guidelines recommend choosing zero-calorie or very low-calorie drinks. This includes:
- Water
- Unsweetened teas
- Coffee with no added sugar
- Diet soda
- Other low-calorie drinks and drink mixes
You can also try flavoring your water with a squeeze of lemon or lime juice for a light, refreshing drink with some flavor. All of these drinks provide minimal calories and carbohydrates.
If you choose to drink juice, be sure the label says it is 100% juice with no sugar added. Juice provides a lot of carbohydrates in a small portion, so be sure to count it in your meal plan. Usually, about 4 ounces or less of juice contains 15 grams of carbohydrates and 50 or more calories.
Avoid sugary drinks like regular soda, fruit punch, fruit drinks, energy drinks, sweet tea, and other sugary drinks. These will raise blood glucose and can provide several hundred calories in just one serving! See for yourself:
- One 12-ounce can of regular soda has about 150 calories and 40 grams of carbohydrates. This is the same amount of carbohydrate in 10 teaspoons of sugar!
- One cup of fruit punch and other sugary fruit drinks have about 100 calories (or more) and 30 grams of carbohydrates.
Work with a registered dietitian or certified diabetes educator on a meal plan that is right for you. You can find a registered dietitian by asking your doctor for a referral or visiting www.eatright.org/find-an-expert. You can also find an ADA-recognized diabetes self-management education program in your area at www.diabetes.org/findaprogram.
All right, guys, that is it for now for the ADA diet or American Diabetes Association Diet. I hope Healthsoothe answered any questions you had concerning the ADA diet or American Diabetes Association Diet.
Feel free to contact us at contact@healthsoothe.com if you have further questions to ask or if there’s anything you want to contribute or correct to this article. And don’t worry, Healthsoothe doesn’t bite.
You can always check our FAQs section below to know more about the ADA diet or American Diabetes Association Diet. And always remember that Healthsoothe is one of the best health sites out there that genuinely cares for you. So, anytime, you need trustworthy answers to any of your health-related questions, come straight to us, and we will solve your problem(s) for you.
Frequently Asked Questions Related to the ADA diet or American Diabetes Association Diet
How Many Carbs Does the American Diabetes Association Recommend?
130 grams: The Recommended Dietary Allowance (RDA) for carbs is 130 grams per day. This number is based on the amount of carbohydrate that is required to provide the brain with adequate glucose.
What Foods to Avoid if Your A1C is High?
- Fried meat.
- Higher-fat cuts of meat, such as ribs.
- Pork bacon.
- Regular cheeses.
- Poultry with skin.
- Deep-fried fish.
- Deep-fried tofu.
- Beans prepared with lard.
Why is my Blood Sugar so High When I'm not eating any Carbs?
So, people reduce their carb intake, go on a low carbohydrate diet, and focus on eating healthy fats and (in many cases) too much protein. But what this solution crucially fails to address is insulin resistance, which is the true cause of those high blood glucose numbers.
What Brings A1C Down Fast?
Go easy on the sweets and sugary beverages, white bread, potatoes, pasta, starchy vegetables, and other carbohydrate-rich foods as these increase your blood sugar levels. Instead, opt for foods that are high in fiber, fruits and vegetables, small servings of lean meats and poultry, and low-fat milk or cheese.
I Am odudu abasi a top-notch and experienced freelance writer, virtual assistant, graphics designer and a computer techie who is adept in content writing, copywriting, article writing, academic writing, journal writing, blog posts, seminar presentations, SEO contents, proofreading, plagiarism/AI checking, editing webpage contents/write-ups and WordPress management.
My work mantra is: “I can, and I will”
Additional resources and citations
- 1https://healthjade.net/what-is-the-american-diabetes-association-ada-diet/
- 2https://diabetes.org/healthy-living/recipes-nutrition
- 3https://www.diabetesfoodhub.org/articles/ask-the-experts-what-is-the-ada-diet.html
The content is intended to augment, not replace, information provided by your clinician. It is not intended nor implied to be a substitute for professional medical advice. Reading this information does not create or replace a doctor-patient relationship or consultation. If required, please contact your doctor or other health care provider to assist you to interpret any of this information, or in applying the information to your individual needs.

