A subcutaneous injection is administered beneath the skin's surface, specifically into the layer of subcutaneous fat located beneath the epidermis and dermis, which house sweat glands and hair follicles. This region serves as the site for subcutaneous injections. The provided resource from Great Ormond Street Hospital (GOSH) offers insights into subcutaneous injections, their necessity, and instructions for administering them to children.
It serves as a refresher for the training provided at GOSH. Three primary devices are utilized for subcutaneous injections at GOSH: a conventional syringe, auto-injector, and pen device. This document primarily focuses on syringe usage for injections. Instructions for using auto-injectors and pen devices are included in their packaging, and our nurses will instruct you on their safe utilization.
How to do a subcutaneous injection
To administer a subcutaneous injection, individuals should adhere to the following steps:
- Select a fatty area of the body such as the abdomen, back of the arm, or thigh. If multiple injections are needed or if injections are administered daily, rotate the injection sites to allow each area to recover between injections.
- Prior to cleaning the area with an alcohol pad, wash hands thoroughly. Ensure the area is completely dry before proceeding to the next step.
- Remove the cap from the needle. Draw the prescribed medication into the syringe as per the instructions on the vial. This typically involves inverting the vial and retracting the plunger to draw in the medication. Gently tap the syringe to eliminate air bubbles.
- Pinch a fold of skin, approximately 2 inches thick, between the thumb and a finger.
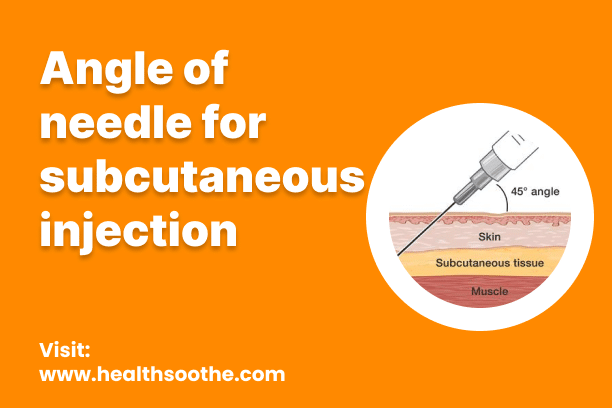
- Holding the needle like a dart, insert it into the skin at a 90-degree angle. Subcutaneous injection needles are typically short and small and should penetrate the skin entirely.
- Depress the plunger swiftly until it reaches the bottom. Avoid applying excessive force.
- Once the injection is complete, cover the needle and dispose of it in a needle-safe container.
The ideal injection site for a subcutaneous injection varies depending on an individual's pain sensitivity and the presence of subcutaneous fat. Commonly chosen locations include the backs or sides of the arms, the fatty part of the stomach, the front of the thighs, and the top of the buttocks where there is more fat than muscle.
Some subcutaneous injections are available in the form of auto-injectors, which are self-contained devices that do not require pre-drawing of the medication. Users can refer to the instructions provided with the auto-injector for proper usage.
Read Also: Understanding Cerebral Palsy Cases and Medical Negligence
Does a subcutaneous injection hurt?
The needle typically utilized for subcutaneous injections is small and short, resulting in minimal discomfort.
The level of pain experienced varies based on several factors, including the injection site, individual pain tolerance, and skin sensitivity. Additionally, the type of medication being injected can contribute to sensations such as stinging, burning, or aching during or after the injection.
Compared to intramuscular injections, subcutaneous injections are generally less painful due to their smaller needles and reduced tissue penetration.
However, children and individuals with needle phobia may still experience anxiety and discomfort during these injections.
Several strategies can help alleviate pain and anxiety:
- Apply a numbing cream to the injection site a few minutes before the procedure, which many doctor's offices offer.
- Use ice to numb the area for a few minutes before the injection.
- Allow nursing babies to breastfeed during injections, which can provide comfort and distraction.
- When restraining a child, opt for a comforting hug rather than holding them down or using a stern approach.
- Offer a pacifier to babies before the injection to soothe them.
- Encourage coughing or blowing before or during the injection to distract from the discomfort.
- Take five deep breaths or guide children to breathe deeply before the injection to promote relaxation.
- Engage in distractions such as watching a movie, playing a video game, or having a conversation. Sometimes, focusing on the injection can exacerbate the sensation of pain.
Pros and Cons of subcutaneous
Pros:
- Convenience
- Absorption Rate
- Avoidance of First-pass Metabolism
- Reduced Risk of Tissue Damage
Cons:
- Limited Volume
- Injection Site Reactions
- Risk of Infection
Differences Between subcutaneous and dimetapp
Subcutaneous Administration:
Subcutaneous administration refers to a method of delivering medication directly into the layer of tissue beneath the skin known as the subcutaneous tissue.
Dimetapp:
Dimetapp is a brand name for a medication that is commonly used to relieve symptoms of allergies, hay fever, and the common cold.
Alternative to subcutaneous
Intramuscular
Intramuscular injections are commonly used for certain vaccines, antibiotics, hormonal medications, and some types of pain management drugs. The choice between subcutaneous and intramuscular administration depends on factors such as the specific medication being administered, the desired rate of absorption, and patient factors such as muscle mass and overall health status.
Are there any complications?
The most common complication following a subcutaneous injection is experiencing pain near the injection site for 1 to 2 days afterward.
Pain around the injection site may occur if the needle is inserted at the wrong angle or if it shifts slightly during the injection process. Some medications can also lead to bruising or irritation at the injection site.
Less frequent complications include:
- Infection: Any break in the skin can permit bacteria to enter, potentially causing an infection. Properly cleaning the injection site and consistently using a fresh needle can help mitigate the risk of infection.
- Contaminated needle: Reusing or sharing needles can facilitate the transmission of diseases from one individual to another. It is crucial to dispose of used needles in a designated container to prevent contamination.
- Injection into a blood vessel: If blood is observed in the syringe, it may indicate inadvertent injection into a blood vessel. This can alter the absorption pattern of the medication. While injecting into a blood vessel can lead to serious complications in rare cases, the likelihood of hitting a blood vessel within subcutaneous fat is extremely low. In most instances, observed blood is likely due to minor bleeding following the injection.
Conclusion
While subcutaneous injections are generally safe and effective methods for administering medication, they can sometimes lead to discomfort and complications. Pain near the injection site is the most common issue, often resolving within a day or two. However, this discomfort can be exacerbated by factors such as incorrect needle insertion or medication properties.
Less common complications include the risk of infection from improper needle handling and the potential for injecting medication into a blood vessel, though the latter is extremely rare within subcutaneous fat.
Despite these risks, proper technique, including site rotation and thorough cleaning procedures, can minimize the likelihood of complications. Additionally, employing strategies to alleviate pain and anxiety, such as numbing creams and distraction techniques, can enhance the overall injection experience.
Ultimately, while subcutaneous injections offer valuable therapeutic benefits, it's essential to prioritize patient safety and comfort by adhering to best practices and addressing any concerns promptly. With careful attention to technique and patient needs, subcutaneous injections can continue to serve as an important treatment modality across various medical settings.
My name is Wisdom Bassey, I’m a blog content writer and graphic designer who provides support and services for brands and different companies. I’m young and versatile, A tech enthusiast. I carry out deep research on every topic I choose to write about. You can reach me through my social media handles, I’m always available and ready to connect.
The content is intended to augment, not replace, information provided by your clinician. It is not intended nor implied to be a substitute for professional medical advice. Reading this information does not create or replace a doctor-patient relationship or consultation. If required, please contact your doctor or other health care provider to assist you to interpret any of this information, or in applying the information to your individual needs.