Before Proceeding, What Do You Know About the Appendix? – Function of the Appendix
[ninja_tables id=”73111″]
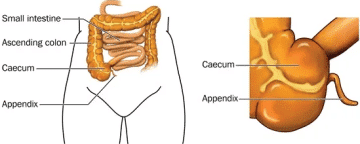
The appendix is a fingerlike pouch attached to the large intestine in the lower right area of the abdomen, the area between the chest and hips. The large intestine is part of the body’s gastrointestinal (GI) tract. The GI tract is a series of hollow organs joined in a long, twisting tube from the mouth to the anus.
The movement of muscles in the GI tract, along with the release of hormones and enzymes, helps digest food. The appendix does not appear to have a specific function in the body, and removing it does not seem to affect a person’s health.
The inside of the appendix is called the appendiceal lumen. Normally, mucus created by the appendix travels through the appendiceal lumen and empties into the large intestine. The large intestine absorbs water from stool and changes it from a liquid to a solid form.
The appendix is a tiny pouch that connects the gut to the stomach. Bacteria may grow within your appendix if it gets obstructed. This might result in the creation of pus and edema, resulting in unpleasant pressure on your belly. Appendicitis[mfn]Appendicitis. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/appendicitis. Accessed September 30, 2022.[/mfn] may potentially cause a blockage in blood flow.
Appendicitis, if left untreated, may end up causing your appendix to erupt. This may allow germs to enter the cavity of your abdomen, which can be dangerous and even deadly.
Introduction and Overview of Appendicitis

Appendicitis occurs due to the inflammation of the appendix – a finger-shaped pouch on the lower right of your belly that extends from your colon.
Pain in the lower right part of your abdomen is caused by appendicitis. In most patients, however, discomfort starts from around the navel and progresses. Appendicitis discomfort normally develops as the inflammation progresses and finally becomes severe.
Although appendicitis may affect anybody, it most often affects individuals aged between 10-30. The appendix is often removed surgically.
Appendicitis occurs when your appendix gets inflamed, most frequently as a result of a blockage. It may be either acute or chronic.
Appendicitis is the leading prevalent cause of stomach discomfort that requires surgery in the United States. It affects up to 9% of Americans at some time in their life.
The appendix is a tiny pouch that connects the gut to the stomach. It’s in your lower right abdomen. Bacteria may grow within your appendix if it gets obstructed. This might result in the creation of pus and edema, resulting in unpleasant pressure on your belly. Appendicitis may potentially cause a blockage in blood flow.
Appendicitis, if left untreated, may end up causing your appendix to erupt. This may allow germs to enter the cavity of your abdomen, which can be dangerous and even deadly.
Types of Appendicitis
Acute appendicitis
This type of appendicitis is a serious case of appendicitis that occurs suddenly. It is more frequent in young people and children aged 10 to 30 years old. It is more common in men than in women. Over the course of 24 hours, pain tends to build and escalate swiftly.
It needs rapid medical attention. It might burst your appendix if left untreated[mfn]Smink D, et al. Management of acute appendicitis in adults. https://www.uptodate.com/contents/search. Accessed September 30, 2021.[/mfn]. This is a potentially deadly problem.
Acute appendicitis is more prevalent than chronic appendicitis, affecting 7 to 9 % of all Americans at some point in their lives.
Chronic appendicitis
Acute appendicitis[mfn]Surgical removal of the appendix. American College of Surgeons. https://www.facs.org/education/patient-education/patient-resources/operations. Accessed September 30, 2021.[/mfn] is more prevalent than chronic appendicitis. It affects only approximately 1.5 percent of persons who have previously experienced chronic appendicitis.
Chronic appendicitis symptoms might be mild and are considered to emerge after an episode of acute appendicitis. Symptoms may fade for a few weeks, months, and even years before reappearing.
This form of appendicitis might be difficult to identify. It is often not detected until it has progressed to acute appendicitis.
Chronic appendicitis is hazardous. Learn all you need to know about recognizing and treating this illness.
What are the Symptoms of Appendicitis?
Appendicitis may cause the following signs and symptoms:
- Pain that starts on the right part of your abdomen and spreads
- Pain that originates from your navel and often moves to the lower right abdomen
- Pain that intensifies with coughing, walking, or other jarring motions
- Vomiting and nausea
- Low-grade fever (below 100 degrees F)
- Fever of low intensity that may develop as the infection progresses
- Diarrhea or constipation
- Abdominal pain or tenderness that hurts more when you cough, sneeze, inhale or move
- Bloating in the abdomen
- Loss of appetite (not feeling hungry when you usually would)
- Flatulence
Pain location may vary based on age and the positioning of the appendix. Because the appendix is higher in women during pregnancy, the pain may appear to emanate from the upper abdomen while you’re pregnant.
Avoid using laxatives or having an enema if you’re constipated and fear you have appendicitis. These therapies have the possibility of causing your appendix to rupture.
If you feel discomfort in the right part of your abdomen coupled with any of the other symptoms of appendicitis, see your doctor.
Appendicitis may rapidly escalate into a medical emergency. If you or your kid, or someone you know develops appendicitis symptoms, call their doctor very soon.
What Causes Appendicitis?
Appendicitis is most commonly caused by an obstruction in the appendix lining, which leads to infection. The germs proliferate quickly, inflaming, swelling, and filling the appendix with pus. The appendix might burst if not treated immediately.
The specific etiology of appendicitis is uncertain in many situations. It is believed to arise when a section of the appendix gets clogged or blocked.
Many factors may obstruct your appendix, including:
- Hardening of the stool
- Expanded lymphoid follicles
- Abdominal injury or trauma
- Digestive tract infection.
- Inflammatory bowel disease.
- Growths inside the appendix
- Intestinal worms
- Severe damage
- Tumors
Abdominal discomfort may be caused by a variety of medical diseases.
Anyone may get appendicitis. However, some individuals may be more prone to developing this ailment than others. Appendicitis risk factors include:
- Age: Appendicitis is more common among teenagers and persons in their twenties, although it may happen at any age.
- Sex: Males are more likely than females to get appendicitis.
- A family history: People with a family background of appendicitis are more likely to develop it.
Complications due to Appendicitis
Appendicitis may lead to significant consequences if the appendix ruptures, allowing feces and germs to enter your abdominal cavity. A burst appendix may cause a variety of unpleasant and sometimes fatal illnesses, including Peritonitis, abscesses, and sepsis.
Your doctor may recommend antibiotics, surgery, or other treatments to prevent or control problems. In certain circumstances, therapy may cause adverse effects or difficulties.
However, the hazards of medicines and surgery are significantly less prevalent and typically less severe than the dangers of untreated appendicitis.
Peritonitis
When your appendix ruptures and germs enter the cavity of the abdomen, the abdominal lining, known as the peritoneum, may become inflamed and infected. This is referred to as peritonitis. It may be very dangerous, even lethal.
Peritonitis symptoms may include high fever, quick pulse, shortness of breath, rapid breathing, and intense and unending stomach discomfort. Medications and surgical procedures to get rid of the appendix are used in treatment.
Abscesses
This is a painful pus-filled pocket that develops around a ruptured appendix. These WBCS are your body’s effort to combat illness. Antibiotics are required to treat the infection, and the abscess must be drained.
During surgery, drainage may occur. Alternatively, the abscess would be drained with a needle prior to surgery. You’ll be sedated, and your physician will guide the surgery through a CT scan, ultrasound, and imaging.
Sepsis
Bacteria from a burst abscess may move through your blood to other regions of your body in rare situations. Sepsis is the medical term for this potentially dangerous disorder. Sepsis symptoms include: Confusion due to a high or low temperature, acute drowsiness, and shortness of breath
According to the Sepsis Alliance, sepsis is a life-threatening emergency that kills one out of every three individuals. Call 911 or your emergency care provider right away if you fear you have sepsis.
Appendicitis may also result in significant consequences such as:
- An appendix rupture: Infection spreads throughout your abdomen as a result of a rupture (peritonitis). This potentially fatal illness requires prompt surgery to extract the appendix and clean your abdominal cavity.
- A pus-filled pouch that arises in the abdomen: If your appendix ruptures, you may have an infection pocket (abscess). A surgeon would usually drain the abscess by inserting a catheter through the wall of your abdomen into the abscess.
The tube stays in place for roughly two weeks, and antibiotics are administered to eliminate the infection. Once the infection has been cleared, you will have an operation to extract the appendix.
Diagnosis of the Appendicitis
Your doctor will most likely collect a record of your symptoms and signs and inspect your belly to help diagnose appendicitis.
Appendicitis is diagnosed using the following tests and procedures:
- Physical examination to determine the source of your discomfort: Gentle pressure upon that sore location may be applied by your doctor. Appendicitis discomfort typically worsens whenever the pressure is abruptly lifted, indicating that the neighboring peritoneum is irritated. Your doctor may also examine you for abdominal tightness and a tendency to tense your abdominals in reaction to pressure on the infected appendix (guarding). Your doctor may inspect your lower rectum with a greased, gloved finger (digital rectal exam). Women of reproductive age may be offered a pelvic examination to rule out any gynecological issues that may be causing the discomfort.
Responses that may indicate appendicitis include:
- Rovsing’s sign: A health care provider tests for Rovsing’s sign by applying hand pressure to the lower left side of the abdomen.
 Pain felt on the lower right side of the abdomen upon the release of pressure on the left side indicates the presence of Rovsing’s sign.
Pain felt on the lower right side of the abdomen upon the release of pressure on the left side indicates the presence of Rovsing’s sign. - Psoas sign: The right psoas muscle runs over the pelvis near the appendix. Flexing this muscle will cause abdominal pain if the appendix is inflamed.
 A health care provider can check for the psoas sign by applying resistance to the right knee as the patient tries to lift the right thigh while lying down.
A health care provider can check for the psoas sign by applying resistance to the right knee as the patient tries to lift the right thigh while lying down. - Obturator sign: The right obturator muscle also runs near the appendix. A health care provider tests for the obturator sign by asking the patient to lie down with the right leg bent at the knee.
 Moving the bent knee left and right requires flexing the obturator muscle and will cause abdominal pain if the appendix is inflamed.
Moving the bent knee left and right requires flexing the obturator muscle and will cause abdominal pain if the appendix is inflamed. - Guarding: Guarding occurs when a person subconsciously tenses the abdominal muscles during an exam. Voluntary guarding occurs the moment the health care provider’s hand touches the abdomen.
 Involuntary guarding occurs before the health care provider actually makes contact and is a sign the appendix is inflamed.
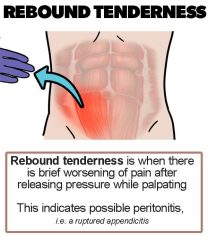
Involuntary guarding occurs before the health care provider actually makes contact and is a sign the appendix is inflamed. - Rebound tenderness: A health care provider tests for rebound tenderness by applying hand pressure to a person’s lower right abdomen and then letting go.
 Pain felt upon the release of the pressure indicates rebound tenderness and is a sign the appendix is inflamed. A person may also experience rebound tenderness as pain when the abdomen is jarred—for example, when a person bumps into something or goes over a bump in a car.
Pain felt upon the release of the pressure indicates rebound tenderness and is a sign the appendix is inflamed. A person may also experience rebound tenderness as pain when the abdomen is jarred—for example, when a person bumps into something or goes over a bump in a car.
- Blood test: This enables your physician to check for infection by looking for an elevated white blood cell count. Your doctor may request a full blood count to look for symptoms of infection (CBC).
 To do this testing, they will take a blood sample and submit it to a laboratory for examination. Bacterial infection is often associated with appendicitis. A urinary tract infection or even other abdominal organ infection may potentially induce symptoms similar to appendicitis. A C-reactive protein testing may also be ordered by your doctor to rule out other reasons for stomach inflammation, like an autoimmune illness or another chronic ailment.
To do this testing, they will take a blood sample and submit it to a laboratory for examination. Bacterial infection is often associated with appendicitis. A urinary tract infection or even other abdominal organ infection may potentially induce symptoms similar to appendicitis. A C-reactive protein testing may also be ordered by your doctor to rule out other reasons for stomach inflammation, like an autoimmune illness or another chronic ailment.
- Urine analysis:
 Your doctor may order a urinalysis to rule out a kidney stone or a urinary tract/bladder infection as the source of your discomfort.
Your doctor may order a urinalysis to rule out a kidney stone or a urinary tract/bladder infection as the source of your discomfort. - Pregnancy test: Ectopic pregnancy can be mistaken for appendicitis. It happens when a fertilized egg implants itself in a fallopian tube, rather than the uterus. This can be a medical emergency. If your doctor suspects you might have an ectopic pregnancy, they may perform a pregnancy test.
To conduct this test, they will collect a sample of your urine or blood. They may also use a transvaginal ultrasound to learn where the fertilized egg has been implanted.
- Pelvic exam: If you were assigned female at birth, your symptoms might be caused by pelvic inflammatory disease, an ovarian cyst, or another condition affecting your reproductive organs. To examine your reproductive organs, your doctor may perform a pelvic exam.
 During this exam, they will visually inspect your vagina, vulva, and cervix. They will also manually inspect your uterus and ovaries. They may collect a sample of tissue for testing.
During this exam, they will visually inspect your vagina, vulva, and cervix. They will also manually inspect your uterus and ovaries. They may collect a sample of tissue for testing.
- Chest imaging tests: Pneumonia in the lower right lobe of your lungs can also cause symptoms similar to appendicitis.
 If your doctor thinks you might have pneumonia, they will likely order a chest X-ray. They may also order an ultrasound or a CT scan to create detailed images of your lungs. Compared to an ultrasound, a CT scan creates more detailed images of your organs. However, there are some health risks associated with radiation exposure from a CT scan, so it’s usually only recommended after an ultrasound and MRI. CT scans can harm a developing fetus. If you’re of childbearing age, your doctor will offer a pregnancy test first.
If your doctor thinks you might have pneumonia, they will likely order a chest X-ray. They may also order an ultrasound or a CT scan to create detailed images of your lungs. Compared to an ultrasound, a CT scan creates more detailed images of your organs. However, there are some health risks associated with radiation exposure from a CT scan, so it’s usually only recommended after an ultrasound and MRI. CT scans can harm a developing fetus. If you’re of childbearing age, your doctor will offer a pregnancy test first.
- Abdominal Imaging examinations: An abdominal X-ray, magnetic resonance imaging (MRI), abdominal ultrasound, or computed tomography (CT) scan may also be recommended by your doctor to assist diagnose appendicitis or rule out other reasons for your discomfort. To check for inflammation of your appendix, your doctor might order imaging tests of your abdomen. This can help check for signs of inflammation, an abscess, or other problems with your appendix. It can also help doctors identify other potential causes of your symptoms, such as:
a. abdominal abscess
b. fecal impaction
c. inflammatory bowel disease
Your doctor may order one or more of the following imaging tests:
- Abdominal ultrasound: Ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. The transducer can be moved to different angles to make it possible to examine different organs.
 In abdominal ultrasound, the health care provider applies gel to the patient’s abdomen and moves a handheld transducer over the skin. The gel allows the transducer to glide easily, and it improves the transmission of the signals. The procedure is performed in a health care provider’s office, an outpatient center, or a hospital by a specially trained technician, and the images are interpreted by a radiologist—a doctor who specializes in medical imaging; anesthesia is not needed. Abdominal ultrasound creates images of the appendix and can show signs of inflammation, a burst appendix, a blockage in the appendiceal lumen, and other sources of abdominal pain. Ultrasound is the first imaging test performed for suspected appendicitis in infants, children, young adults, and pregnant women.
In abdominal ultrasound, the health care provider applies gel to the patient’s abdomen and moves a handheld transducer over the skin. The gel allows the transducer to glide easily, and it improves the transmission of the signals. The procedure is performed in a health care provider’s office, an outpatient center, or a hospital by a specially trained technician, and the images are interpreted by a radiologist—a doctor who specializes in medical imaging; anesthesia is not needed. Abdominal ultrasound creates images of the appendix and can show signs of inflammation, a burst appendix, a blockage in the appendiceal lumen, and other sources of abdominal pain. Ultrasound is the first imaging test performed for suspected appendicitis in infants, children, young adults, and pregnant women. - Abdominal CT scan: CT scans use a combination of x-rays and computer technology to create three-dimensional (3-D) images. For a CT scan, the person may be given a solution to drink and an injection of contrast medium. CT scans require the person to lie on a table that slides into a tunnel-shaped device where the x-rays are taken. The procedure is performed in an outpatient center or a hospital by an x-ray technician, and the images are interpreted by a radiologist; anesthesia is not needed. Children may be given a sedative to help them fall asleep for the test.
 A CT scan of the abdomen can show signs of inflammation, such as an enlarged appendix or an abscess—a pus-filled mass that results from the body’s attempt to keep an infection from spreading—and other sources of abdominal pain, such as a burst appendix and a blockage in the appendiceal lumen. Women of childbearing age should have a pregnancy test before undergoing a CT scan. The radiation used in CT scans can be harmful to a developing fetus.
A CT scan of the abdomen can show signs of inflammation, such as an enlarged appendix or an abscess—a pus-filled mass that results from the body’s attempt to keep an infection from spreading—and other sources of abdominal pain, such as a burst appendix and a blockage in the appendiceal lumen. Women of childbearing age should have a pregnancy test before undergoing a CT scan. The radiation used in CT scans can be harmful to a developing fetus. - Abdominal MRI scan: MRI machines use radio waves and magnets to produce detailed pictures of the body’s internal organs and soft tissues without using x-rays. The procedure is performed in an outpatient center or a hospital by a specially trained technician, and the images are interpreted by a radiologist. Anesthesia is not needed, though children and people with a fear of confined spaces may receive light sedation, taken by mouth. An MRI may include the injection of a special dye, called contrast medium. With most MRI machines, the person lies on a table that slides into a tunnel-shaped device that may be open-ended or closed at one end; some machines are designed to allow the person to lie in a more open space. An MRI can show signs of inflammation, a burst appendix, a blockage in the appendiceal lumen, and other sources of abdominal pain. An MRI used to diagnose appendicitis and other sources of abdominal pain is a safe, reliable alternative to computerized tomography (CT) scan.
- Abdominal X-ray: The using of an x-ray machine to test for appendicitis, whereby rays are used to scan your abdomen any abnormalities detected is shown in the x-ray screen.
 In some cases, you might need to stop eating food for a period of time before your test. Your doctor can help you learn how to prepare for it.
In some cases, you might need to stop eating food for a period of time before your test. Your doctor can help you learn how to prepare for it.
If your doctor believes you have appendicitis, doctors will discuss your findings and medical history with you. They’ll next undertake a physical examination to look for soreness in your lower right abdomen, as well as edema or stiffness. A digital rectal examination may also be performed.
Your doctor may prescribe one or more tests to look for evidence of appendicitis or to rule out other possible explanations of your symptoms based on the findings of your physical exam.
There is no one test that can be used to diagnose appendicitis. If your doctor is unable to find any other explanations for your symptoms, appendicitis may be diagnosed.
Treatment of Appendicitis
Appendicitis is often treated with surgery to extract the inflamed appendix. Antibiotics may be used prior to surgery to treat the infection. The following are ways appendicitis is treated:
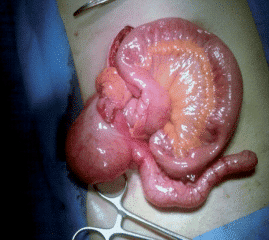
- Appendix removal surgery (appendectomy): Appendectomy[mfn]Appendectomy. Surgical removal of the appendix. American College of Surgeons. https://www.facs.org/education/patient-education/patient-resources/operations. Accessed September 30, 2021.[/mfn] may be done as an open procedure with a single abdominal incision of two to four inches (5 to 10 cm) in length (laparotomy). There are two methods for this type of surgery, and both have a low risk of complications.
- Open appendectomy:
 During this common procedure, a surgeon makes up to a four-inch incision on the lower right-hand side of the belly to remove the patient’s appendix
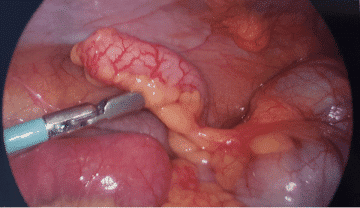
During this common procedure, a surgeon makes up to a four-inch incision on the lower right-hand side of the belly to remove the patient’s appendix - Laparoscopic appendectomy:
 During this cutting-edge, less invasive surgery, a surgeon makes up to three tiny incisions in the patient’s belly and then inserts a special device to remove the appendix; typically causes less pain and scarring
During this cutting-edge, less invasive surgery, a surgeon makes up to three tiny incisions in the patient’s belly and then inserts a special device to remove the appendix; typically causes less pain and scarring
- Laparoscopic surgery: Alternatively, the procedure might be performed via a few minor incisions of the abdomen (laparoscopic surgery).
 The surgeon puts sophisticated surgical equipment and a video recorder into your belly during laparoscopy to remove your appendix. Laparoscopic surgery, in general, enables you to recover quicker and recover with much less pain and scars. It may be preferable for elderly folks and obese persons. However, laparoscopic surgery is not for everyone. If your appendix has burst and infection has gone beyond the appendix, or if there is an abscess, your surgeon may recommend an open appendectomy to clear the abdominal cavity.
The surgeon puts sophisticated surgical equipment and a video recorder into your belly during laparoscopy to remove your appendix. Laparoscopic surgery, in general, enables you to recover quicker and recover with much less pain and scars. It may be preferable for elderly folks and obese persons. However, laparoscopic surgery is not for everyone. If your appendix has burst and infection has gone beyond the appendix, or if there is an abscess, your surgeon may recommend an open appendectomy to clear the abdominal cavity.
After your appendectomy, you should be prepared to spend either 1 or 2 days in the hospital.
- Draining an abscess prior to appendectomy:
 If the appendix has ruptured and an abscess has developed around it, then the abscess may be emptied by inserting a tube into the abscess via your skin. After the infection has been controlled, an appendectomy may be done several weeks later.
If the appendix has ruptured and an abscess has developed around it, then the abscess may be emptied by inserting a tube into the abscess via your skin. After the infection has been controlled, an appendectomy may be done several weeks later. - Laparotomy:
 Laparotomy removes the appendix through a single incision in the lower right area of the abdomen.
Laparotomy removes the appendix through a single incision in the lower right area of the abdomen.
Can Appendicitis be Treated without Surgery?
Nonsurgical treatment may be used if surgery is not available, a person is not well enough to undergo surgery, or the diagnosis is unclear. Nonsurgical treatment includes antibiotics to treat the infection.
How Can I Prevent Appendicitis?
There’s no sure way to prevent appendicitis. But you might be able to lower your risk of developing it by eating a fiber-rich diet. Although more research is needed on the potential role of diet, appendicitis is less common in countries where people eat high-fiber diets.
Foods that are high in fiber include:
- fruits
- vegetables
- lentils, split peas, beans, and other legumes
- oatmeal, brown rice, whole wheat, and other whole grains
- Your doctor may also encourage you to take a fiber supplement.
How Common is Appendicitis?
Approximately 5% of Americans will develop appendicitis. It’s the No. 1 cause of abdominal pain requiring surgery.
Who Might Get Appendicitis?
Appendicitis can occur at any age, although it’s most common in people in their teens and 20s. Appendicitis in children most often occurs during the tween or teen years. But even elementary school-age children get appendicitis.
What if the Surgeon finds a Normal Appendix?
Occasionally, a surgeon finds a normal appendix. In this case, many surgeons will remove it to eliminate the future possibility of appendicitis. Occasionally, surgeons find a different problem, which may also be corrected during surgery
What to Do After an Appendectomy
After your appendectomy, your physician will prescribe drugs to help you manage your discomfort. When combined with your prescriptions, several complementary and alternative therapies may help reduce pain. Discuss with your doctor regarding safe alternatives, such as:
Distracting activities that keep your mind off your discomfort, like listening to songs and conversing with friends. With youngsters, distraction may be extremely beneficial. Simply close your eyes and imagine a beloved spot as an example of guided imagery.
After an appendectomy, you should expect to be out of commission for a few weeks, or much longer if your appendix burst. To assist your body in healing, do the following:
- First, avoid strenuous activity. If the appendectomy was performed laparoscopically, you should rest for 3-5 days. Restrict your activities for 10 to 14 days after an open appendectomy. Always consult your doctor about activity restrictions and when you can continue routine functions after surgery.
- When you cough, keep your abdomen supported. To help relieve pain, position a pillow on top of your abdomen and exert pressure before coughing, laughing, or moving.
- If your meds aren’t working, consult your doctor. Pain puts additional strain on your body and hinders the healing process. Call your doctor if you are still in pain after taking pain relievers.
- When you’re ready, get up and move. Begin softly and gradually increase your activities when you feel ready. Begin with short walks.
- When you’re exhausted, sleep. As your body recovers, you may find yourself sleeping more than normal. Take it gently and relax as necessary.
- Consult your doctor about going back to work or school. You may return to work whenever you are ready. Children might be able to go back to school in less than a week. They should rest for 2 to 4 weeks before engaging in strenuous physical activity, like gym/fitness classes or sports.
Does Removing the Appendix Have any Side Effects? – What are the dangers of removing the appendix?
The appendix does not appear to have a specific function in the body, and removing it does not seem to affect a person’s health.
When Should You Visit a Doctor?
Arrange an appointment with your doctor if either you or your kid is experiencing any concerning signs or symptoms of appendicitis. Severe abdominal pain needs prompt medical treatment.
Getting ready for your appointment
If you are experiencing abdominal discomfort, see your primary care physician. If you suffer from appendicitis, you will almost certainly be hospitalized and sent to a surgeon to have your appendix removed.
What you are able to do
When you book the appointment, ask whether there is anything you need to do ahead of time, like fasting before a certain test. Make a list of the following:
- Your symptoms, including those that seem to be unrelated to the cause of your visit
- Important personal information, such as substantial life pressures, recent life changes, and family medical histories
- All drugs, vitamins, and other supplements you use, as well as the dosages.
What to discuss with your doctor
If possible, bring a friend or family member with you to assist you to recall the facts. Some fundamental questions you should ask your doctor about appendicitis include:
- Is this appendicitis?
- Will I have to take any further tests?
- Other than appendicitis, what else may I have?
- Do I need surgery, and if so, when?
- What are the dangers of removing the appendix?
- How long will I have to remain in the hospital after the surgery?
- How long will it take to recover?
- When can I return to work following surgery?
- Can you detect if my appendix has ruptured?
- Please do not be afraid to ask further questions.
What to anticipate from your doctor
Your doctor will most likely ask you numerous questions, including:
- When did your stomach ache start?
- Where does it cause pain?
- Has the ache shifted?
- How bad is your pain?
- What makes your discomfort worse?
- What helps you get rid of your pain?
- Have you got a fever?
- Do you get a nauseating feeling?
- What are your other indications and symptoms?
A Note from Healthsoothe
Without prompt medical attention, appendicitis can be quite serious. A ruptured appendix causes a widespread infection that can be deadly.
See your healthcare provider if you have severe abdominal pain, a key sign of appendicitis. Your provider can rule out other causes.
Appendicitis sometimes goes away with antibiotics alone. If you need surgery, a minimally invasive laparoscopic approach uses small incisions to help you recover faster.
All right, guys, that is it for now for appendicitis. I hope Healthsoothe answered any questions you had concerning appendicitis.
Feel free to contact us at contact@healthsoothe.com if you have further questions to ask or if there’s anything you want to contribute or correct to this article. And don’t worry, Healthsoothe doesn’t bite.
You can always check our FAQs section below to know more about appendicitis.
And always remember that Healthsoothe is one of the best health sites out there that genuinely cares for you.
[bwla_faq faq_topics=”frequently-asked-questions-about-appendicitis” sbox=”1″ paginate=”1″ pag_limit=”5″ list=”1″ /]

I Am odudu abasi a top-notch and experienced freelance writer, virtual assistant, graphics designer and a computer techie who is adept in content writing, copywriting, article writing, academic writing, journal writing, blog posts, seminar presentations, SEO contents, proofreading, plagiarism/AI checking, editing webpage contents/write-ups and WordPress management.
My work mantra is: “I can, and I will”


 Pain felt on the lower right side of the abdomen upon the release of pressure on the left side indicates the presence of Rovsing’s sign.
Pain felt on the lower right side of the abdomen upon the release of pressure on the left side indicates the presence of Rovsing’s sign.  A health care provider can check for the psoas sign by applying resistance to the right knee as the patient tries to lift the right thigh while lying down.
A health care provider can check for the psoas sign by applying resistance to the right knee as the patient tries to lift the right thigh while lying down. 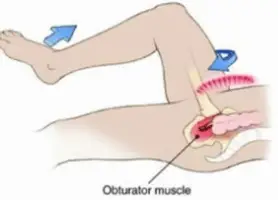 Moving the bent knee left and right requires flexing the obturator muscle and will cause abdominal pain if the appendix is inflamed.
Moving the bent knee left and right requires flexing the obturator muscle and will cause abdominal pain if the appendix is inflamed. 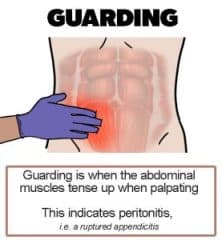

 Your doctor may order a urinalysis
Your doctor may order a urinalysis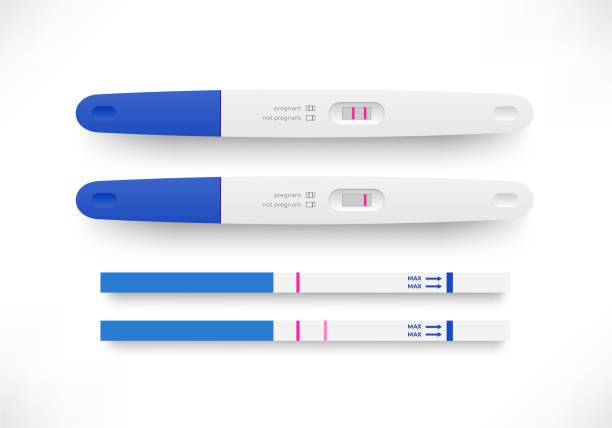 To conduct this test, they will collect a sample of your urine or blood. They may also use a transvaginal ultrasound to learn where the fertilized egg has been implanted.
To conduct this test, they will collect a sample of your urine or blood. They may also use a transvaginal ultrasound to learn where the fertilized egg has been implanted.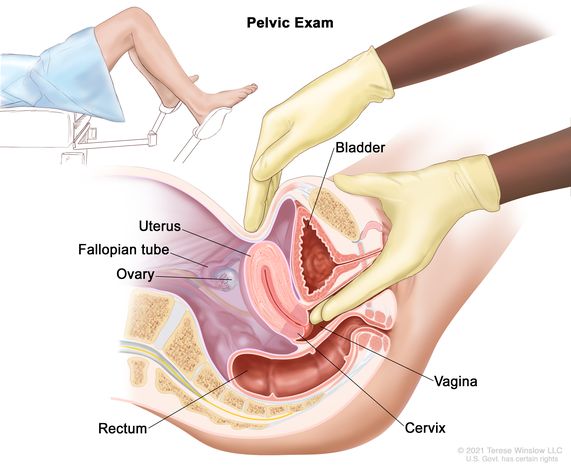 During this exam, they will visually inspect your vagina, vulva, and cervix. They will also manually inspect your uterus and ovaries. They may collect a sample of tissue for testing.
During this exam, they will visually inspect your vagina, vulva, and cervix. They will also manually inspect your uterus and ovaries. They may collect a sample of tissue for testing.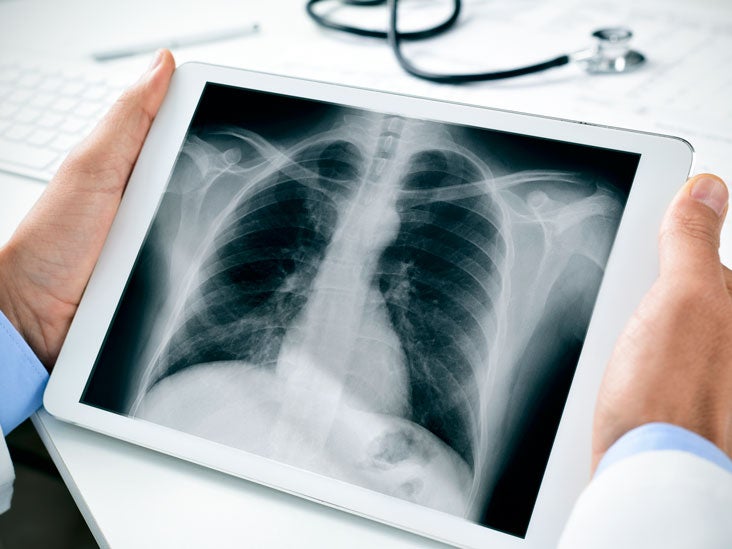

 A CT scan of the abdomen can show signs of inflammation, such as an enlarged appendix or an abscess—a pus-filled mass that results from the body’s attempt to keep an infection from spreading—and other sources of abdominal pain, such as a burst appendix and a blockage in the appendiceal lumen. Women of childbearing age should have a pregnancy test before undergoing a CT scan. The radiation used in CT scans can be harmful to a developing fetus.
A CT scan of the abdomen can show signs of inflammation, such as an enlarged appendix or an abscess—a pus-filled mass that results from the body’s attempt to keep an infection from spreading—and other sources of abdominal pain, such as a burst appendix and a blockage in the appendiceal lumen. Women of childbearing age should have a pregnancy test before undergoing a CT scan. The radiation used in CT scans can be harmful to a developing fetus.
 During this common procedure, a surgeon makes up to a four-inch incision on the lower right-hand side of the belly to remove the patient’s appendix
During this common procedure, a surgeon makes up to a four-inch incision on the lower right-hand side of the belly to remove the patient’s appendix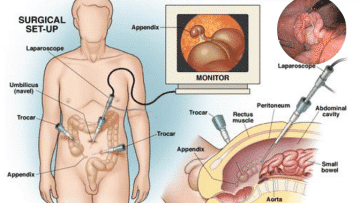 During this cutting-edge, less invasive surgery, a surgeon makes up to three tiny incisions in the patient’s belly and then inserts a special device to remove the appendix; typically causes less pain and scarring
During this cutting-edge, less invasive surgery, a surgeon makes up to three tiny incisions in the patient’s belly and then inserts a special device to remove the appendix; typically causes less pain and scarring The surgeon puts sophisticated surgical equipment and a video recorder into your belly during laparoscopy to remove your appendix.
The surgeon puts sophisticated surgical equipment and a video recorder into your belly during laparoscopy to remove your appendix. 
