Share this post
What is Avascular Necrosis?
Avascular necrosis occurs as a result of dead bone tissue due to a lack of blood supply. Also called osteonecrosis, aseptic necrosis, or ischemic bone necrosis, over time, the bone becomes tiny and can lead to breakage of the bones and the bone's eventual collapse.
A broken bone or dislocated joint can interfere with the blood flow to a section of bone condition. Avascular necrosis is also linked with long-term use of high-dose steroid medications and excessive alcohol intake.
Avascular necrosis occurs mostly in the hip. Other common parts of the body are the shoulder, knees, shoulder, and ankles. Any individual can be affected, but the condition is most common in people between the ages of 30 and 50.
Symptoms of Avascular Necrosis
When to see a doctor
Seek medical attention if you have constant pain or pain that refuse to go away in any joint. See your doctor immediately if you think you have a broken bone or a dislocated joint.
Causes of avascular necrosis
- Joint or bone trauma. An injury, such as a dislocated joint, might damage nearby blood vessels. Cancer treatments associated with radiation also can reduce bone strength and affect blood vessels.
- Fatty deposits in blood vessels. The fat (lipids) block the small blood vessels decrease the blood flow that feeds bones.
- Certain diseases. Medical conditions, such as sickle cell anemia and Gaucher's disease, also contribute to diminished blood flow to the bone.
Risk factors for developing avascular necrosis
- Trauma. Injuries, such as hip dislocation or fracture, can damage nearby blood vessels and reduce blood flow to bones.
- Steroid use. Use of high-dose corticosteroids, such as prednisone, is a common cause of avascular necrosis. The reason is unknown, but one hypothesis is that corticosteroids can increase lipid levels in your blood, reducing blood flow.
- Excessive alcohol use. If you are the type that consumes a lot of alcoholic drinks per day for so many years can also cause fatty deposits to produce in your blood vessels.
- Bisphosphonate use. Using bisphosphate medications for so many years to increase bone density might contribute to developing osteonecrosis of the jaw. This rare complication has occurred in some individual patient treated with high doses of these medications for cancers, such as multiple myeloma and metastatic breast cancer.
- Certain medical treatments. Radiation therapy for cancer can lessen bone. Organ transplantation, especially kidney transplant, also is linked with avascular necrosis.
Medical conditions associated with avascular necrosis include:
- Pancreatitis
- Diabetes
- Gaucher's disease
- HIV/AIDS
- Systemic lupus erythematosus
- Sickle cell anemia
Complications of developing Avascular necrosis
Prevention of Avascular necrosis
- Reduce your alcohol intake. Excessive drinking is one of the major factors for developing avascular necrosis.
- Keep your cholesterol levels calm low. Little bits of fat is a very common substance that does block blood supply to bones.
- Monitor your steroid use. Inform your doctor about your past and present use of long-term high-dose steroids. Steroid-related bone damage appears to worsen with repeated courses of high-dose steroids.
- Don't smoke at all. If you smoke you are at risk of developing the condition.
Diagnosis of avascular necrosis
Imaging tests
Many disorders can cause joint pain. Imaging tests can help pinpoint the source of pain. Options include:
- X-rays. They can reveal bone changes that occur in the later stages of avascular necrosis. In the condition's early stages, X-rays usually appear normal.
- MRI and CT scan. These tests produce detailed images that can show early changes in bone that might indicate avascular necrosis.
- Bone scan. A small amount of radioactive material is injected into your vein. This tracer travels to the parts of your bones that are injured or healing and shows up as bright spots on the imaging plate.
Treatment for Avascular Necrosis
The goals of treatment for AVN are to improve or prevent further bone loss of the affected joint, stop further bone damage, and ease the pain.
The best treatment will depend on a number of factors, including:
- Your age
- Stage of the disease
- Location and amount of bone damage
- Cause of Avascular Necrosis (AVN)
If avascular necrosis is detected early, treatment includes taking medications to ease pain or reduce the use of the affected joint. If your hip, knee, or ankle is affected, crutches may be necessary to take weight off the damaged joint. Your doctor may also recommend range-of-motion exercises to help keep the affected area mobile.
While these nonsurgical treatments may slow the progression of avascular necrosis, most people with the condition eventually need surgery. Your doctor might recommend:
- Nonsteroidal anti-inflammatory drugs. Medications, such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve) might help relieve the pain associated with avascular necrosis.
- Osteoporosis drugs. Medications, such as alendronate (Fosamax, Binosto), might reduce the further process of the avascular necrosis, but no concrete evidence that supports the claim or mixed evidence
- Cholesterol-lowering drugs. Lowering drugs might help prevent the vessel blockages by reducing the amount of cholesterol and fat in your blood that can cause avascular necrosis.
- Electrical stimulation. Electrical currents might encourage your body to grow new bone to replace the damaged bone. And it can be administered through electrodes attached to your skin.
Because most people don't develop symptoms earlier until avascular necrosis become severe at an advanced stage, your doctor might recommend surgery. Surgical options include:
- Bone grafts, these surgeries involve extracting removing healthy bone from one part of the body to the other damaged bone joint.
- Osteotomy, which involves cutting the bone and replace its alignment to ease stress on the joint
- Total joint replacement, the procedure involves extracting the damaged bone or joint and replacing it with a synthetic joint
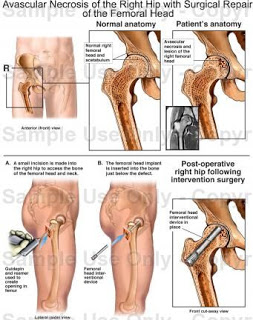
- Core decompression, which involves extracting some part inside of the bone to ease the pressure. After, new blood vessels form.
- Vascularized bone graft, which involves using the individual own tissue to rebuild damaged hip joints; the surgeon first removes the bone with the poor blood supply from the hip and then replaces it with the blood-vessel-rich bone from another site, such as the fibula, the smaller bone located in the lower leg.
- Regenerative medicine treatment. Bone marrow aspirate and concentration is a newer procedure that might be appropriate for early-stage avascular necrosis of the hip. It involves removing the dead hip bone and Stem cells inserted in its place, which allows new bone to form. More study is needed.
Your family doctor might refer you to a doctor who specializes in disorders of the joints (rheumatologist) or to an orthopedic surgeon.
What you can do
Make a list of:
- Your symptoms, including any that may seem unrelated to the reason why you scheduled the appointment, and when they began
- Key medical information, including other conditions you have any history of injury to the painful joint
- All medications, vitamins or other supplements you take, including doses
Some questions to ask your doctor about avascular necrosis include:
- What's the most likely cause of my symptoms?
- What tests do I need?
- What treatments are available?
- I have other health conditions. How can I best manage them together?
What to expect from your doctor
- Where's your pain?
- Does a particular joint position make the pain better or worse?
- Have you ever taken steroids such as prednisone?
- How much alcohol do you drink?
RELATED READING
- What is Osteomyelitis and how does it enter the bone?
- Why a Healthy Mouth Is Good For Your Body
- What You Should Know About Osteonecrosis of the Jaw
- Ischemic Heart Disease: Symptoms, Causes, Treatment and Prevention

Isreal olabanji a dental assistant and public health professionals and has years of experience in assisting the dentist with all sorts of dental issues.
We regularly post timely and trustworthy medical information and news on Fitness, Dental care, Recipes, Child health, obstetrics, and more.
