A blown vein indicates a vein that has burst and is dripping blood. When a nurse or other healthcare expert tries to inject a needle into a vein, something doesn't go quite as planned, it occurs. Your skin will discolour around the insertion site as the vein begins to leak. The needle has to be taken out after that.
That vein cannot be used for IV line insertion, blood draws, or medicine injections until it has had time to recover. In this article, we'll examine the causes, symptoms, and treatment options for blown veins.
What are the primary symptoms of a blown vein?
Once you have a blown vein, discolouration will probably show up quite rapidly. Additional signs include:
- tenderness or mild pain around the injection site
- stinging
- bruising
- Swelling
Blood can no longer flow freely through a collapsed vein because it has been blasted and has caved in. Upon the reduction of the edema, blood flow will restart. That vein can't be utilised right now.
A collapsed vein may be permanent if the damage is severe enough.
What can cause a blown vein?
When a needle enters a vein and exits through the opposite side, the vein is ruptured. This may occur for a number of reasons.
Using an inadequate-sized needle
Both veins and needles come in a variety of diameters. A nurse must select the ideal vein from those that are available and determine the appropriate needle size for that vein.
Tell your nurse if you've ever experienced issues with any particular veins and how they were finally resolved.
incorrect angle or "fishing"
Slowly and at the correct angle, without going too shallow or deep, a needle must be inserted. Blowing a vein can happen when you're off the mark.
It's crucial to avoid moving the needle around in search of another vein if a vein cannot be inserted on the first try. The needle needs to be removed and reinserted in a more suitable spot.
swishing veins
Different veins have varying degrees of thickness and toughness. This type of vein can roll or bounce as the medical professional tries to inject it.
The vein may be punctured by the needle, but it may not go all the way in before the vein rolls and bursts.
during insertion, moving
A blown vein could occur if you move even slightly while the needle is being inserted. That’s why it’s important to relax your arm and stay as still as you can until the needle is all the way in and the healthcare provider has loosened the tourniquet.
Long-term IV drug use
IV drug use can damage veins and cause scar tissue to form, which can be permanent. This can happen if you have a health problem that requires frequent use of IV drugs (for example, if you’re receiving chemotherapy for cancer and you don’t have a chemo port).
It can also happen if you have a substance abuse problem and use needles. In addition to the repeated needle insertion that can blow veins, the substance you’re injecting can contribute to blown veins. For example, research from trusted Sources shows that heroin’s acidity can damage veins.
In time, accessing functioning veins can become problematic.
Age
As we age, we start losing tissue beneath our skin, and our veins become more fragile and less stable. They can roll around under the skin during IV insertion, increasing the risk of blowing a vein.
How is a blown vein treated?
You have a blown vein if needle insertion causes swelling and bruising. Although it might hurt and feel uncomfortable, it is completely safe.
To reduce blood loss and swelling, the healthcare professional typically applies a little pressure to the injection site. To avoid infection, they clean the area after a short while.
An ice pack can ease symptoms in cases of severe swelling.
For a day or two, you might feel a little uncomfortable. Within a few days, the bruise should begin to fade, and it should be gone entirely in 10 to 12 days.
How to prevent a blown vein
If you're well-hydrated, finding a nice vein will be simpler. Before having blood drawn or getting an IV inserted, be sure to drink lots of fluids unless otherwise instructed, such as before surgery. Any prior vein issues should be disclosed to your doctor.
Because they want to avoid damaging a vein, your healthcare practitioner is taking their time getting ready to put the needle. By maintaining complete stillness during the needle's entry, you may assist.
If you're afraid of needles, turn around and concentrate on taking slow, deep breaths until it's finished.
Your medical professional should take the time to:
- Pick a vein that is straight, visible, and of a decent size for the surgery.
- Steer clear of where veins converge. They should ask you to create a fist if it's difficult to locate a vein.
- Use a tourniquet or another tool to draw attention to the vein. A blood pressure cuff may be preferred to a tourniquet for elderly people. A tourniquet should not be applied too tightly.
- Select the appropriate needle for the vein.
- At an angle of no more than 30 degrees, insert the needle.
- Applying a thumb below the point of penetration will stabilise the vein.
- Take a methodical, slow approach.
- The tourniquet must be released before the needle may be removed.
- Remove the needle with caution, then gently press the area.
Ultrasound or other imaging tools are helpful when it's difficult to locate the proper vein. Even with the utmost care, blown veins may still occur.
What are the potential complications of a blown vein?
A blown vein often only results in a minor injury and is not a significant issue. But until the vein has healed, it's crucial that it not be utilised again.
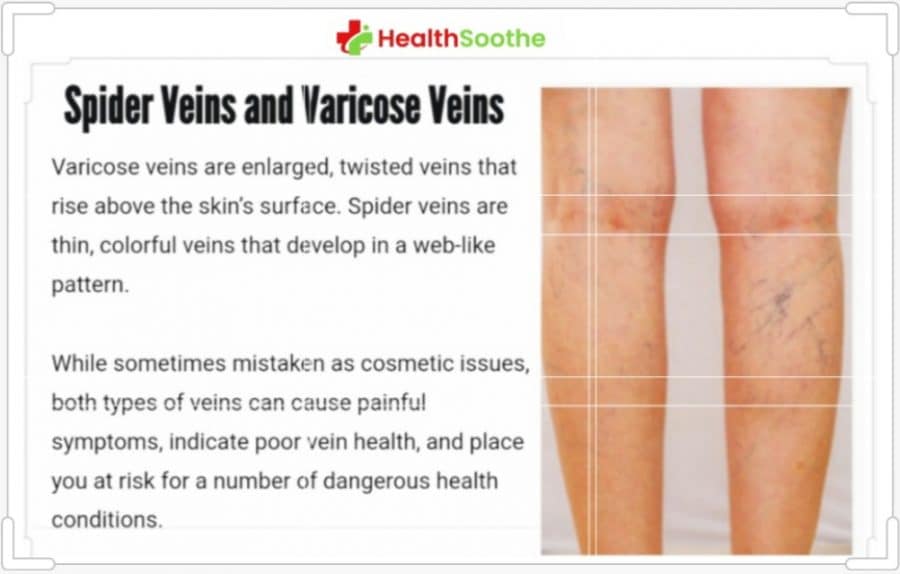
A blown vein may sometimes collapse and stop the flow of blood. While some collapsed veins may recover, others never do. Depending on where the vein lies, this may result in circulation issues. The collapsing vein will be bypassed by newly formed blood channels.
When medicine intended for intravenous administration leaks onto the skin, it may sometimes be dangerous. When that occurs, more medical care could be needed.
Conclusion:
When a vein is pierced by a needle and bursts, it is said to have been "blown." Even though it might sting and bruise, most minor injuries heal on their own in a matter of days.