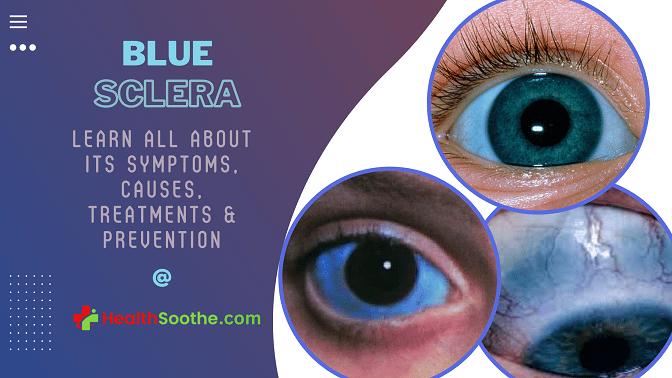
There are people in this world whose sclera (the whitish of the eye) is blue. Like really? Why would the part of the eyes that is always white naturally be blue in some people? Most people wonder about this, and if you are here, you are probably on this list.
[ninja_tables id=”73259″]
What you see is known as ‘blue sclera’, Ever heard of it? Did you look in the mirror, and found out that the whitish part of your eye is now bluish, and wondered what it is? This condition is known as blue sclera.
Most people having this condition (blue sclera) are always scared and really worried that this is an indication that they are going blind, but this is not the case. In this article, Healthsoothe aims to explain all there is to know about blue sclera; what are its symptoms? What causes it? How can you prevent and treat blue sclera?
Alright, let’s move.
Blue Sclera – What is it?

Blue sclera is a condition in which the white part of the eye (sclera) has a blue, gray, or purplish tint. In many cases, blue tint in the sclera occurs as a symptom of an underlying condition, or as a reaction to a specific medication. The blue tint is generated by the sclera’s collagen fibers being thin and transparent, enabling veins in the deeper tissues to show through.
One or both eyes may have a bluish sclera, and it’s usually not painful. Depending on the cause, blue in the whites of the eyes may be visible at birth or may become noticeable later on in life.
Having a blue sclera is relatively harmless and has no cause for alarm. However, it could be a symptom of a more serious underlying condition. If you notice a sudden change in sclera color, see an eye doctor. They can examine your eyes, determine the cause and offer treatment options.
Blue sclerae are seen in various illnesses, notably connective tissue disorders. These include, among other things, Ehlers-Danlos syndrome, Marfan’s syndrome, Willems De Vries syndrome, pseudoxanthoma elasticum, and osteogenesis imperfecta (OI).
Blue sclera is produced by the sclera’s collagen fibers being thin and transparent, allowing the vision of the basal uvea. In congenital illnesses such as osteogenesis imperfecta (OI), the sclera, the white outer layer of the eye that surrounds the iris, may be weakened.
Several connective tissue disorders are associated with the blue sclera, including Ehlers-Danlos syndrome, Marshall and Stickler syndrome, Willems De Vries syndrome, Marfan syndrome, POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal protein, and skin changes) syndrome, pseudoxanthoma elasticum, and, brittle cornea syndrome to name a few.
Juvenile Paget’s disease, Diamond-Blackfan anemia, acid phosphatase deficiency, and severe iron deficiency anemia are also on the list of bone and blood problems. Severe types of osteogenesis imperfecta (OI) are usually detected in childhood, although minor examples may not be discovered until later in adulthood.
The basal choroidal veins that show through the sclera give the sclera its blue-gray tint. Because the faulty type I collagen is not developing properly, the sclera is thinner than usual. The sclera is a thick, weakly vascularized connective tissue structure made up of collagen types I, III, IV, V, VI, and VIII, as well as elastin, proteoglycans, and glycoproteins.
The prevalence of osteogenesis imperfecta in the United States is estimated to be one in every 20,000 live births. In the United States, osteogenesis imperfecta affects between 20,000 and 50,000 persons. Individuals with osteogenesis imperfecta are conceived with deficient connective tissue or the inability to produce it, often because of a Type I collagen shortage.
The amino acid replacement of glycine to bulkier amino acids in the collagen triple helical structure causes this deficit. As a consequence, the body may react by hydrolyzing the faulty collagen structure. If the body does not remove the abnormal collagen, the link between the hydroxyapatite crystals and collagen fibrils that form bone is disrupted, resulting in brittleness.
Osteogenesis imperfecta[mfn]Das S, Bhatnagar K. Blue sclera and osteogenesis imperfect – A rare association. Kerala J Ophthalmol. 2017;29:240–3. [Google Scholar][/mfn] has long been thought to be an autosomal dominant Type I collagen disease. The majority of cases have been linked to morphisms in the COL1A2 and COL1A1 genes. The discovery of autosomal recessive types has occurred in recent years.
At least seven subgroups have been identified, with four primary sub-types ranging from moderate to severe. People with Type I osteogenesis imperfecta have minor bone deformation, persistent blue sclera, close to normal height by maturity, and a greater-than-half likelihood of hearing loss.
Patients with perinatal fatal (Type II) osteogenesis imperfecta have the most severe symptoms, including many fractures in utero or during birth. These patients are generally stillborn or die young. The intensity of osteogenesis imperfecta is determined by the particular gene deficiency.
The majority of instances of osteogenesis imperfecta are transmitted from one’s parents. Some occurrences, however, are the consequence of new genetic alterations. A person who has osteogenesis imperfecta does have a 50% probability of transferring the gene and the illness to their offspring.
A 16-year-old boy was referred to a department in a hospital for ruling out a metabolic bone disorder. He presented to the emergency with an elbow fracture due to a fall on an outstretched hand. He denied a history of recurrent fractures, deafness, skeletal deformities, and dentition abnormalities.
His past medical history was otherwise normal and none of the immediate family members had a history of fractures. Systemic examination was unremarkable except for the fracture olecranon process on the right side. An ophthalmic examination revealed a bluish sclera involving the right eye.
His visual acuity, the field of vision, color vision, pupillary reflexes, and extraocular movements were normal in both eyes. Skeletal survey and markers of bone metabolism were normal. He was diagnosed with a case of idiopathic unilateral bluish sclera and was kept under follow-up.
The bluish sclera is associated with osteogenesis imperfecta, Marfan’s syndrome, Ehlers-Danlos syndrome, blue sclera syndrome (Van der Heave syndrome), incontinentia pigmenti, and many other inherited conditions. The sclera is involved bilaterally in all these conditions and the unilateral appearance is a rarity.
Unilateral bluish sclera is reported earlier with nevus depigmentosus, familial, and idiopathic in origin. The bluish hue of the sclera is due to the thinning of the collagen fibers and increased transparency which exposes the underlying uvea.
The bluish sclera, therefore, is seen in many conditions with defective type 1 collagen formation. Osteogenesis imperfecta is the classical condition associated with the bluish sclera.
However, our patient did not have any features to suggest the same. It is essential to screen for musculoskeletal and connective tissue abnormalities in patients with the blue sclera.
What are the Symptoms of Blue Sclera?
Blue sclera is characterized by a blue color of the sclera and may be caused by a pathologic or non-pathologic reason. Myopia, epicanthal fold, angioid streaks, keratoconus, and thin cornea are further visual features of connective tissue diseases linked with blue sclera.
Kyphoscoliosis, heart abnormalities, brittle bones, joint hypermobility, vascular abnormalities, hearing abnormalities, gastrointestinal abnormalities, and skin abnormalities are all systemic features of connective tissue diseases linked with the blue sclera.
What Causes Blue Sclera?
The sclera is a thick connective tissue made up of different types of collagen and proteins. It works as a protective layer and extends from the cornea at the front of the eye, to the optic nerve at the back of the eye.
In a healthy eye, the sclera is white and smooth, and so what are blue sclera causes? When a sclera has a bluish tint, it’s often caused by thinning of the sclera. Thinness or transparency of scleral tissue makes the uvea, located beneath the sclera, and blood vessels more visible.
Essentially the blue tint in the white part of the eye is really the layers below the sclera peeking through the tissue.
Causes of scleral thinning often have to do with conditions that affect bone or connective tissue development. Other causes include anemia or similar iron deficiencies, certain medications, and exposure to silver compounds.
Blue sclera is the most common appearance of osteogenesis imperfecta (OI), which is caused by a mutation in the COLIA1 and COL1A2 genes, which code for type I procollagen. However, categories of this ailment (types IV-VI) with normal sclerae have been discovered. Osteogenesis imperfecta is also linked to defective bone fragility and hearing.
Brittle cornea syndrome is characterized by the blue sclera, red hair, and brittle cornea, as well as skeletal, skin, and dental problems. A missense variation in ZNF469 has already been identified as the cause of illness.
Cornea plana, pseudoxanthoma elasticum, buphthalmos, keratoconus, peripheral sclerocornea, high myopia, keratoglobus[mfn]Imamoglu S, Kaya V, Imamoglu EY, Gok K. Congenital keratoglobus with blue sclera in two siblings with overlapping Marshall/Stickler phenotype. Indian J Ophthalmol. 2016;64(11):856-859. doi:10.4103/0301-4738.195615 [/mfn], oculodermal melanocytosis, ciliary/equatorial staphyloma, microcornea, and Ehlers-Danlos syndrome are other underlying conditions associated with the formation of the blue sclera.
Blue sclera is a rare complication of Turner syndrome, Marfan syndrome, pyknodysostosis, Cheney syndrome, Hallermann-Streiff syndrome, Menkes syndrome, ectodermal dysplasia, or brittle corneas.
Normal newborns may also have blue sclera during the first few months of life; however, the persistence of blue discoloration over time may indicate the existence of increased intraocular pressure.
Premature newborns, especially those of Caucasian heritage, typically have blue sclerae. Blue sclera could also be inherited as an autosomal dominant/autosomal recessive abnormality.
Conditions Associated With a Bluish Sclera
Usually if a child is born with blue sclera, it’s due to a genetic disorder that affects the scleral tissue. Below are some conditions — both genetic and acquired — that could contribute to a blue sclera:
- Osteogenesis imperfecta
Blue sclera in a patient with osteogenesis imperfecta. The most common cause of blue sclera is osteogenesis imperfecta, otherwise known as brittle bone disease. It’s a genetic condition caused by a mutation in the gene that produces collagen.
Collagen is a key part of building strong bones. Because the sclera is also made of collagen, a lack of it — or having collagen that doesn’t work as it should — causes the sclera to be weaker or thinner than normal.
There are different types of osteogenesis imperfecta. The types categorize the varying symptoms presented and their severity. People with the disease have bones that are weak and, in some cases, misshapen.
- Anemia or iron deficiency
Someone with chronically low iron levels can experience a bluish tint to the sclera. This can affect adults, as well as babies who are born with low iron. Iron is an important part of the collagen production process.
Studies found that collagen development is actually impaired when iron levels are low. When collagen isn’t being produced normally, it can cause the sclera (which is made of collagen) to thin and weaken.
- Oculodermal melanocytosis (ODM)
Also known as nevus of Ota, this condition is characterized by excessive pigmentation in the uvea, sclera, episclera, and eyelids. This results in a bluish-gray tint in the sclera and eyelids.
While this condition is not dangerous at face value, having it significantly increases one’s risk of developing uveal melanoma. In fact, experts look at ODM as a precursor to uveal melanoma.
If you’ve been diagnosed with ODM, it’s critical that you protect your eyes from UV exposure and get regular eye exams to manage the health of your eyes.
- Marfan syndrome
Like many other conditions associated with blue sclera, Marfan syndrome affects the body’s connective tissue. Connective tissue keeps the organs, cells, and tissues together. It’s relied on heavily for proper growth and development.
In addition to vision problems such as high myopia, exotropia, and other abnormalities, Marfan syndrome can cause the whites of the eyes[mfn]Walsh, S. “The Eyes Have It.” Medscape. [/mfn] to appear blue or gray.
- Pseudoxanthoma elasticum
Though blue sclera is rare[mfn]Jha AK, Sinha R, Prasad S. Nevus depigmentosus with unilateral bluish sclera, a rare entity. Indian Dermatol Online J. 2015;6:358–9. [PMC free article] [PubMed] [Google Scholar][/mfn], it’s possible for a blue sclera to result from pseudoxanthoma elasticum. This is a genetic disease in which elastic body tissue becomes calcified.
The skin and cardiovascular system are usually affected most, as well as the retina. However, cases of blue-tinted scleras have been reported in association with the disease.
- Kabuki syndrome
This is a genetic disorder resulting from a mutation in genes KMT2D and KDM6A. Though the symptoms and their severity vary among those affected, Kabuki syndrome can cause growth delays, skeletal abnormalities, distinctive facial features, and intellectual disability.
Facial features seen in Kabuki syndrome include long openings between the eyelids (palpebral fissures) and a droopy upper eyelid (ptosis). Blue sclera is also a symptom.
- Addison’s disease
Addison’s disease is a rare disorder in which the adrenal gland doesn’t create enough cortisol and aldosterone. These are some of the most important hormones that the body makes.
One of the many symptoms involved with the condition is hyperpigmentation in and around mucus membranes. This often includes the eyes and gums.
- Alkaptonuria
Also known as “Black Urine disease,” Alkaptonuria is a rare disorder that affects the body’s ability to break down tyrosine and phenylalanine. These are two important amino acid proteins. Since the amino acid can’t be broken down, a build-up of homogentisic acid occurs in the body
The build-up of homogentisic acid can cause urine to appear dark and many health problems throughout a person’s life. This includes having grayish-blue or brown spots in the sclera, a blue tint to cartilage in the ear, and issues with the bones and joints.
- Ehlers Danlos syndromes
Ehlers Danlos syndromes is an umbrella term for a collection of genetic disorders that affect the connective tissue. More specifically, these disorders inhibit the production of collagen.
The most common presentation of these disorders is hypermobility (being “double jointed”) and having stretchy or loose skin. Because there’s a lack of collagen production, it’s also common for scleras to be thin. This results in a bluish tint in the sclera.
Medications that can Cause Blue Sclera
Developing blue sclera as an older adult — meaning the condition was acquired — usually means it’s caused by something in your medicine cabinet, not a genetic disease. Below are some medications that have been known to cause a blue tint in the sclera.
Talk to your doctor about the side effects you’re experiencing from your medication. Usually adjusting your dosage or finding an alternative treatment will help resolve the problem.
- Minocycline: Minocycline treats bacterial infections, including pneumonia and urinary tract infections. One of the side effects of this medication is changes in the skin, teeth, gum, and nail color. If someone who is taking this medicine has a blue tint to their sclera, they may also have a blue tint to their nail beds.
- Antipsychotics: Antipsychotics are prescribed to treat certain mental illnesses. These include schizophrenia, bipolar disorder, depression, and certain personality disorders. Phenothiazines, which is a group of antipsychotic medications, may cause blue sclera.
- Amiodarone: Amiodarone is a drug that treats cardiac problems, like arrhythmia (irregular heartbeat). When taking this drug, it’s possible for it to accumulate in the skin. This results in a blue-gray tint on the face, hands, and eyes.
- Phenytoin: Phenytoin is a seizure medication reported to cause blue discoloration of the skin and eyes. Besides blue sclera, patients also have blue nail beds, lips, and conjunctiva. Permanent vision changes were also reported.
- Mitoxantrone: Mitoxantrone is a chemotherapy drug that is administered intravenously. Approximately 10%-29% of patients experience a bluish or greenish discoloration of the sclera and urine after treatment. This side effect usually lasts one to two days after treatment.
Diagnosis and Treatment of Blue Sclera
External inspection, systemic assessment, and slit lamp biomicroscopy for related illnesses are all used to diagnose blue sclera. Although there is no conclusive test for osteogenesis imperfecta, genetic testing may confirm or rule out known mutations.
Blue sclera treatment entails identifying and treating the true cause. Blue sclera is caused mostly by hereditary abnormalities and, to a lesser degree, by non-genetic illnesses, and it may arise as an adverse reaction to treatment.
To mention a few, blue sclerae are often linked with congenital collagen synthesis diseases such as Ehlers-Danlos syndrome, Marfan syndrome, Willems De Vries syndrome, pseudoxanthoma elasticum, and osteogenesis imperfecta.
Juvenile Paget’s disease, severe iron deficiency anemia, acid phosphatase deficiency, and Diamond-Blackfan anemia are also on the list of bone and blood problems. Adults with alkaptonuria, conjunctival melanoma, Addison disease, and ocular melanosis have all been reported to have acquired blue sclerae.
Non-ocular symptoms may need referrals to orthopedic and pediatric specialists. Individuals with blue sclera as well as other symptoms of a systemic illness may benefit from genetic counseling for linked hereditary conditions.
In situations of severe thinning and perforation, surgical treatment may be needed. A conserved scleral graft or autologous fascia lata may give structural support, especially when suturing a device like a tube implant is required. To address underlying pathology, systemic investigations and therapy should be addressed.
There is not yet a cure for this disease. However, specific therapies can reduce the pain and complications from OI. Drugs that can increase the strength and density of bone are called bisphosphonates.
Low-impact exercises, such as swimming, keep muscles strong and help maintain strong bones. People with OI can benefit from these exercises and should be encouraged to do them.
In more severe cases, surgery to place metal rods into the long bones of the legs may be considered. This procedure can strengthen the bone and reduce the risk of fracture. Bracing can also be helpful for some people.
Surgery may be needed to correct any deformities. This treatment is important because deformities (such as bowed legs or a spinal problem) can interfere with a person’s ability to move or walk.
How Do You Prevent Blue Sclera?
Genetic counseling is recommended for couples considering pregnancy if there is a personal or family history of this condition.
Does Blue Sclera Have Any Side Effects – Can You Be Blind Due To Blue Sclera?
Usually, having a sclera with a blue tint is not an immediate threat. Especially if you’ve been diagnosed with a genetic condition in which blue sclera is a symptom. Sudden onset of blue sclera is still no cause for alarm, but an eye exam is recommended.
An eye doctor can take a look and determine the cause of the change. If you have any sudden changes in your vision, like blurriness or light sensitivity, or the whites of your eyes have turned yellow, you need to see a doctor.
You should also see a doctor if the change in scleral color is accompanied by pain, irregular eye discharge or swelling.
As I had earlier said about the 16yr boy who was brought for diagnosis and treatment due to the bluish tint in his eye, which was blue sclera; his visual acuity, the field of vision, color vision, pupillary reflexes, and extraocular movements were normal in both eyes.
Skeletal survey and markers of bone metabolism were normal. He was diagnosed with a case of idiopathic unilateral bluish sclera[mfn]Makwana N, Jagannathan M. Unilateral blue sclera: A diagnostic enigma? Indian J Plastic Surg. 2003;36:139–40. [Google Scholar][/mfn] and was kept under follow-up. So, blue sclera won’t lead to blindness, but rather, it is a symptom of an underlying illness (mostly genetic) which I have listed in this article, and therefore, an eye exam is recommended.
Healthsoothe’s Verdict on Blue Sclera
When to see a doctor: Usually, having a sclera with a blue tint is not an immediate threat. Especially if you’ve been diagnosed with a genetic condition in which blue sclera is a symptom. Sudden onset of blue sclera is still no cause for alarm, but an eye exam is recommended.
An eye doctor can take a look and determine the cause of the change. If you have any sudden changes in your vision, like blurriness or light sensitivity, or the whites of your eyes have turned yellow, you need to see a doctor.
You should also see a doctor if the change in scleral color is accompanied by pain, irregular eye discharge or swelling.
The existence of ocular/systemic symptoms of the underlying illness affects the prognosis. Individuals with blue sclera are more likely to have a globe rupture or scleral perforation following standard eye surgery. Systemic problems such as hearing loss, arterial rupture, bone fractures, and carotid-cavernous fistula are also common in patients.
How well a person does depends on the type of OI (blue sclera) they have;
- Type I, or mild OI, is the most common form. People with this type can live a normal lifespan.
- Type II is a severe form that often leads to death in the first year of life
- Type III is also called severe OI. People with this type have many fractures starting very early in life and can have severe bone deformities. Many people need to use a wheelchair and often have a somewhat shortened life expectancy.
- Type IV, or moderately severe OI, is similar to Type I, although people with Type IV often need braces or crutches to walk. Life expectancy is normal or near normal.
Blue sclera may be associated with multisystem disorders, so good history-taking is most important. The most dreaded complications associated are OI, cardiac abnormalities, and hearing defects.
Osteogenesis imperfecta(OI) is an autosomal disorder, and genetic counseling is recommended for couples considering pregnancy if there is a personal or family history of this condition. Patients should have a multidisciplinary approach to prevent complications as so far no cure for this disorder.
[bwla_faq faq_topics=”frequently-asked-questions-about-blue-sclera” sbox=”1″ paginate=”1″ pag_limit=”5″ list=”1″ /]