The human body is made up of interconnected blood vessels which play an important role in the transportation of blood to organs and tissues. Each of these vessels is unique as they have its specific functions.
Quick Facts About Collapsed Vein
| A | B |
|---|---|
| Definition | A collapsed vein occurs when blood flow is restricted due to inflammation caused by irritation from needles or drugs administered intravenously |
| Causes | Repeated injections, especially with blunt needles; poor injection technique; substances that irritate veins; hypertonic fluids; vasoactive substances; extreme pH fluids; oral liquid methadone |
| Symptoms | Discoloration, swelling, itching, bruising; cold feet or hands due to poor circulation; the vein may disappear into the skin |
| Mechanism | Veins may become temporarily blocked if the internal lining swells in response to injury or irritation. This may be caused by the needle, the substance injected, or donating plasma |
| Prognosis | Swelling may subside and circulation could be re-established. However, some collapsed veins may never recover and the body may create smaller veins that are inadequate for injections or IVs |
| Diagnosis | Physical examination, ultrasound, venography, or angiography |
| Prevention | Using proper injection techniques, rotating injection sites, using sharp needles, and avoiding substances that irritate veins can help prevent vein collapse |
| Treatment | Treatment involves resting the affected vein, applying warm compresses, and in some cases, medical intervention may be necessary |
| Compliactions | Poor circulation can increase the risk of stroke, cardiovascular problems, and kidney disease. Cyanosis, a bluish discoloration of the skin, can occur due to inadequate oxygenation of the blood |
The vein is the blood vessel that returns deoxygenated blood from organs and tissues in the body back to the heart. The vein closest to the skin’s surface is often used as a medium for drug administration and venipuncture.
But what happens when you have a collapsed vein? Do you know what a collapsed vein means? Well, if you haven’t or you have, and still wanna know more about it, then you are in the right place - Healthsoothe.
In this article, we’ll look into the causes and symptoms of a collapsed vein, as well as how it can be prevented. So read on.
Definition of a Collapsed Vein

A vein collapses when there is a restriction of blood flow in the vein as a result of an inflammation caused by irritation from the needle or drugs administered intravenously.
It could be temporary or permanent depending on the cause and management. If temporary, once the swelling reduces, blood circulation resumes.
Watch the video below to know more on collapsed vein:
What are the Signs and Symptoms of a Collapsed Vein - What do Collapsed Veins Look Like?
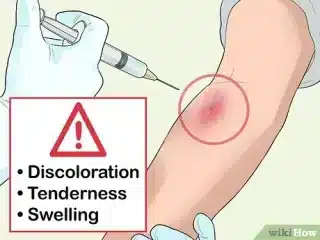
You may notice discoloration almost quickly in the area of the collapsed vein. Swelling, itching, and bruising are also cold feet or hands due to poor blood circulation.
You can’t determine if a vein has collapsed just by looking at your skin. The collapse happens underneath the skin, inside the vein. A vein that has collapsed has no blood going through it, and sometimes the vein itself disappears into the skin, blending into the surrounding area.
Causes of Collapsed Vein

A vein collapses as a result of a serious injury in the vein usually because of using the same vein repeatedly for drug administration, or the administration of drugs that irritates the veins.
It could be a temporary collapse, if allowed to heal, the vein recovers. Sometimes, it could be permanent, such veins really don’t recover. Collapsed veins which usually lead to permanent vein collapse are caused by the following:
- Using the same vein repeatedly
- Using blunt needles
- Wrong intravenous technique
- Removing the needle from the vein too fast
- Injection of substances which irritate the veins; in particular, injection of liquid methadone intended for oral use.
Veins that are smaller may collapse as a result of using too much suction while drawing back against the syringe's plunger to ensure the needle is inserted into the vein.
This will draw the vein's sides together, and if they are irritated, they may cling together, prompting the vein to clog. Similarly, withdrawing the needle too rapidly after injecting might have the same consequence.
What can Lead to Permanent Vein Collapse?

- Using old/blunt needles
- Long-term usage of wrong sizes of needles
- Improper drug administration techniques
- Long-term usage of a particular vein as the only route for drug administration intravenously
- Injecting drugs that irritate the veins.
- Injecting into swollen sites
- Tying a tourniquet too tight
To know more on this, watch the video below:
What are the Potential Complications of a Collapsed Vein?

Most of the time, a collapsed vein is a minor injury, not a serious problem. But it’s important that the vein not be used again until it’s healed.
Sometimes, a collapsed vein can collapse and prevent blood from flowing1Ciccarone D, et al. (2015). Fire in the vein: Heroin acidity and its proximal effect on users’ health. DOI:10.1016/j.drugpo.2015.04.009. Collapsed veins can heal, but some never bounce back. Depending on the location of the vein, this can lead to circulation problems. New blood vessels will develop to bypass the collapsed vein.
When a vein collapses, the body must find another way to pump blood. The circulatory system automatically compensates for the blockage by pumping more blood through surrounding smaller veins. These are known as new veins because they only appear under the skin when a normal vein has been blocked.
Although new veins help to circulate your blood, they are a sign you have permanent damage to your veins. Blood flow is essential to healing, and the long-term impacts of collapsed veins include:
- Long-term numbness, swelling, and discoloration
- Increased risk for infection
- Sores that do not heal
- Ulcers
- Necrosis (skin dies due to blood loss)
In some cases, a medication that was to be delivered intravenously can be potentially harmful when spilled into the skin. When that happens, further treatment may be required.
How to Prevent Collapsed Veins
Prevention is better than cure. It’s safer to prevent collapsed veins and one of the most important ways is to avoid drugs that could irritate your veins. Make sure to do the following:
- Ensure you consult your doctor or pharmacist before any drugs are administered intravenously2Pieper, B., Kirsner, R. S., Templin, T. N., & Birk, T. J. (2007). Chronic Venous Disease and Injection Drug Use. Arch Intern Med., 167(16). https://doi.org/doi:10.1001/archinte.167.16.1807-a.
- When stressed or scared, our veins become invisible. It’s okay to look away from the needle and maintain calm until the process is over.
- When properly hydrated it’s easier to find veins3Staying Hydrated – Staying Healthy. American Heart Association. Retrieved October 15, 2022, from https://www.heart.org/en/healthy-living/fitness/fitness-basics/staying-hydrated-staying-healthy. Ensure you drink enough water before going for an IV injection4Moureau NL. (2008). Tips for inserting an I.V. device in an older adult. DOI: 10.1097/01.NURSE.0000342005.69106.d7 or venipuncture.
- Try to keep calm during needle insertions. If you feel uncomfortable, let your healthcare provider know.
- Avoid using blunt needles.
- Do not inject into any noticed swollen area5World Health Organization. (2010). WHO guidelines on drawing blood: Best practices in phlebotomy. who.int/infection-prevention/publications/drawing_blood_best/en/.
- Your healthcare provider should always use the best vein with the right needles.
- A slow steady approach is safer.
- Proper use of a tourniquet: It should not be too tied.
- The needle should be inserted at 30 degrees or less.
Treatment of Collapsed Vein
A temporarily collapsed vein may heal when the inflammation reduces and the vein is allowed to rest, hence giving it time to heal. Taking vitamin C or consuming fruits rich in vitamin C will hasten the healing process.
A permanently collapsed vein may not heal, and blood flow is shut off from such veins, sometimes the body regenerates new tiny veins to aid blood circulation in that area but they are usually smaller and weaker than the normal veins, making them not so useful for IV drug administration6Pieper, B., Templin, T. N., Kirsner, R. S., & Birk, T. J. (2009). Impact of injection drug use on distribution and severity of chronic venous disorders. Wound repair and regeneration : official publication of the Wound Healing Society [and] the European Tissue Repair Society, 17(4), 485–491. https://doi.org/10.1111/j.1524-475X.2009.00513.x.
It is important to see a phlebologist if you notice any abnormality or difference in your veins.
Collapsed veins are permanent7Roberts, J. R. (2018). A Day in the Life of a Classic Opioid Abuser. Emergency Medicine News, 12–14.. Besides allowing the area to heal and preventing infection, there are no treatments that restore blood flow through the vein.
Scarring inside of the vein is permanent, but there are a few ways that you can speed up the healing process of the vein and the surrounding skin:
- Stop injecting in the area, and move to a different vein8Preston, A., & Derricott, J. (n.d.). The Safer Injecting Handbook. Exchange Supplies. Retrieved October 15, 2022, from https://www.exchangesupplies.org/pdf/P303_9.pdf.
- Keep the area clean, especially while the skin is healing.
- Use anti-inflammatory medications, like ibuprofen, to reduce pain and swelling.
- If the area remains red or swollen, see a doctor for antibiotics to prevent infection.
- Let your vein breathe: One particular vein should not always be used every time9Getting Off Right: A Safety Manual for Injection Drug Users. Harmreduction.Org; National Harm Reduction Coalition. https://harmreduction.org/issues/safer-drug-use/injection-safety-manual/potential-health-injections/. Give your vein time to heal from the hole caused by the piercing. This will reduce the risk of the inflammation that could lead to temporary vein collapse.
You could do a few vein exercises regularly that will make your veins more healthy, visible, and ready to be used. Ensure you talk to your phlebologist before doing any of the exercises.
How Long Does It Take a Collapsed Vein to Heal?
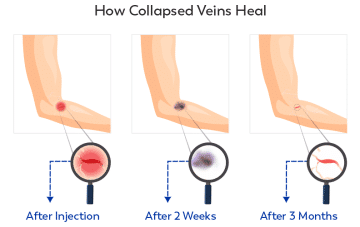
Collapsed veins that heal shut never recover blood flow. Instead, the body compensates by pumping blood through other veins10Haond, C.; Ribreau, C.; Boutherin-Falson, O.; Finet, M. (1999-10-01). "Laminar flow through a model of collapsed veins. Morphometric response of endothelial vascular cells to a longitudinal shear stress non uniform cross-wise". The European Physical Journal Applied Physics. 8 (1): 87–96. Bibcode:1999EPJAP...8...87H. doi:10.1051/epjap:1999233. ISSN 1286-0042..
Bruising, swelling, and scabbing around the injection site will heal if the individual stops using that area to shoot up.
However, the scar tissues that build up inside the vein are permanent, and blood flow may never fully return to what it was before the damage.
Key Takeaways from Healthsoothe
A collapsed vein occurs when a needle punctures through the vein and causes it to rupture. It may sting and bruise, but it’s generally a minor injury that clears up within a few days.
A temporary collapse vein may heal when the inflammation reduces and the vein is allowed to rest, hence giving it time to heal. Taking vitamin C or consuming fruits rich in vitamin C will hasten the healing process.
A permanently collapsed vein may not heal, and blood flow is shut off from such veins, sometimes the body regenerates new tiny veins to aid blood circulation in that area but they are usually smaller and weaker than the normal veins, making them not so useful for IV drug administration.
It is important to see a phlebologist if you notice any abnormality or difference in your veins. Collapsed veins are permanent. Besides allowing the area to heal and preventing infection, there are no treatments that restore blood flow through the vein.
The best thing you can do to prevent further damage to your veins is to address your addiction now. Having a collapsed vein isn’t life-threatening, but over time vein damage accumulates and causes serious health problems.
In the most severe cases, vein damage from drug use leads to life-threatening infections and the loss of a limb.
All right, guys, that is it for now for the collapsed vein. I hope Healthsoothe answered any questions you had concerning a collapsed vein.
Feel free to contact us at contact@healthsoothe.com if you have further questions to ask or if there’s anything you want to contribute or correct to this article. And don’t worry, Healthsoothe doesn’t bite.
You can always check our FAQs section below to know more about the collapsed vein.
And always remember that Healthsoothe is one of the best health sites out there that genuinely cares for you.
Frequently Asked Questions about Collapsed Vein
Can You Get a Collapsed Vein in Your Foot?
Can You Get a Collapsed Vein from Dehydration?
No, being dehydrated does not cause veins to collapse – they are only caused by injections. However, being dehydrated thickens your blood, which can exacerbate vein damage and problems with circulation.
How Do I Get Help for a Collapsed Vein?
Can You Repair Collapsed Veins?
Collapsed veins can sometimes recover on their own. However, a vein that has permanently collapsed will never recover and cannot be repaired, so it's important to avoid causing this issue by seeking treatment.
Additional resources and citations
- 1Ciccarone D, et al. (2015). Fire in the vein: Heroin acidity and its proximal effect on users’ health. DOI:10.1016/j.drugpo.2015.04.009
- 2Pieper, B., Kirsner, R. S., Templin, T. N., & Birk, T. J. (2007). Chronic Venous Disease and Injection Drug Use. Arch Intern Med., 167(16). https://doi.org/doi:10.1001/archinte.167.16.1807-a
- 3Staying Hydrated – Staying Healthy. American Heart Association. Retrieved October 15, 2022, from https://www.heart.org/en/healthy-living/fitness/fitness-basics/staying-hydrated-staying-healthy
- 4Moureau NL. (2008). Tips for inserting an I.V. device in an older adult. DOI: 10.1097/01.NURSE.0000342005.69106.d7
- 5World Health Organization. (2010). WHO guidelines on drawing blood: Best practices in phlebotomy. who.int/infection-prevention/publications/drawing_blood_best/en/
- 6Pieper, B., Templin, T. N., Kirsner, R. S., & Birk, T. J. (2009). Impact of injection drug use on distribution and severity of chronic venous disorders. Wound repair and regeneration : official publication of the Wound Healing Society [and] the European Tissue Repair Society, 17(4), 485–491. https://doi.org/10.1111/j.1524-475X.2009.00513.x
- 7Roberts, J. R. (2018). A Day in the Life of a Classic Opioid Abuser. Emergency Medicine News, 12–14.
- 8Preston, A., & Derricott, J. (n.d.). The Safer Injecting Handbook. Exchange Supplies. Retrieved October 15, 2022, from https://www.exchangesupplies.org/pdf/P303_9.pdf
- 9Getting Off Right: A Safety Manual for Injection Drug Users. Harmreduction.Org; National Harm Reduction Coalition. https://harmreduction.org/issues/safer-drug-use/injection-safety-manual/potential-health-injections/
- 10Haond, C.; Ribreau, C.; Boutherin-Falson, O.; Finet, M. (1999-10-01). "Laminar flow through a model of collapsed veins. Morphometric response of endothelial vascular cells to a longitudinal shear stress non uniform cross-wise". The European Physical Journal Applied Physics. 8 (1): 87–96. Bibcode:1999EPJAP...8...87H. doi:10.1051/epjap:1999233. ISSN 1286-0042.

