Any abnormality of the 1autonomic nervous system is known as dysautonomia (ANS). Your heartbeat, breathing, temperature, digestion, and many other uncontrollable bodily processes are all under the ANS's control.
Fast heartbeats, lightheadedness, or fainting upon rising are typical signs of dysautonomia.
Diabetes, alcohol use disorder, Parkinson's disease, and autoimmune disorders are just a few of the illnesses that can lead to dysautonomia. Genes may also play a role. Doctors occasionally fail to identify the root cause.
The types, causes, symptoms, and diagnoses of dysautonomia will all be covered in this article. Additionally, it will look at resources and treatments for dysautonomia for those with ANS dysfunction.
Read Also: What Does Dysautonomia Feel Like?
What is dysautonomia?
Your ANS may be malfunctioning in whole or in part, which is known as dysautonomia. It is also known as autonomic dysfunction. According to Dysautonomia International, dysautonomia affects more than 70 million people worldwide.
People of any gender or race can experience dysautonomia, which can manifest at any age. It may start later in life or be inherited and present at birth.
A side effect of pregnancy, surgery, physical trauma, or illnesses that harm nerves, like diabetes, Guillain-Barre syndrome, multiple sclerosis, and some infections, is autonomic dysfunction.
Various symptoms may manifest depending on the nerve in question. You might experience an accelerated heartbeat, for instance, if it affects the nerves that control the heart. You might start sweating excessively if it affects the sweat glands.
Some people only experience mild, sporadic symptoms, which may even go away. Others have more severe, persistent, and incapacitating symptoms.
Dysautonomia's underlying cause may be treated to alleviate symptoms. In addition to medication and lifestyle changes, there are treatments for the symptoms themselves. However, dysautonomia is incurable.
What is dysautonomia pots' life expectancy?
Early on, it resembles 2Parkinson's disease in terms of symptoms. However, from the time of diagnosis, persons with this illness often only have a 5 to 10-year life expectancy. It's an uncommon illness that mostly affects individuals over 40.
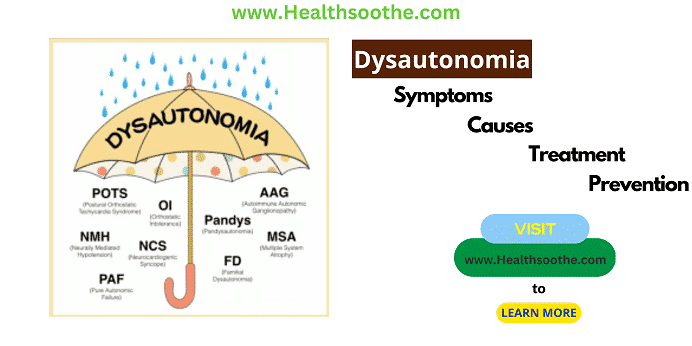
What are the different forms of dysautonomia?
Syndrome of postural orthostatic hypotension (POTS):
Up to 3 million Americans are affected by this type, with young girls or adolescents being the most susceptible. Your heart beats too quickly when you stand up due to the blood flow and circulation issues caused by POTS. Shortness of breath, dizziness, and chest pain may result from this.
Neurally mediated syncope (NMS):
NMS, formerly known as neurocardiogenic syncope, causes blood pressure to decrease when you stand up, which might make you dizzy.
Vasovagal syncope:
a kind of NMS that is susceptible to emotional triggers like pain or fear. Although it may happen to anybody at any age, the condition is more frequent in children and young people. Usually, it runs in families.
Familial dysautonomia:
This genetic condition sometimes referred to as Riley-Day syndrome, is brought on by a mutation in the ELP1 gene. A lack of tears, poor eating, and weak muscular tone are among the symptoms that often manifest in infancy.
Learning difficulties are seen in one-third of affected youngsters. The inability to control body temperature and a reduction in pain sensitivity are other symptoms. People of Eastern European descent, especially Ashkenazi Jews, are most likely to be affected.
Pure autonomic failure (PAF):
PAF typically manifests in people 60 years of age or older. Bradbury-Eggleston syndrome is another name for it. Dizziness, fainting, vision issues, fatigue, and chest pain are all PAF symptoms that are brought on by a sharp drop in blood pressure when standing. In most cases, symptoms disappear when you sit or lie down.
Multiple system atrophy (MSA):
After the age of 40, a rare and potentially fatal form of dysautonomia appears. MSA, also called Shy-Drager syndrome, is a neurodegenerative condition that is fatal 5 to 10 years after diagnosis.
What is postural orthostatic tachycardia syndrome?
POTS is a collection of symptoms that appear while getting up from a seated posture. It may be identified by a sudden rise in heart rate of at least 30 beats per minute (BPM) brought on by shifting the body into an upright posture.
When standing, gravity causes blood volume to be redistributed to the legs and belly, which in turn reduces the amount of blood the heart has to pump in the centre.
While orthostatic hypotension, a related and sometimes concomitant disorder, may cause a dip in blood pressure upon standing, POTS alone is not linked to a drop in blood pressure.
Diagnosing POTS
Similar to my situation, POTS can be challenging to diagnose. This is due to the fact that although the syndrome has a wide range of symptoms, it can present itself slightly differently in each patient.
Before using a tilt table test to measure heart rate while lying down and standing, medical professionals frequently conduct a thorough physical examination and bloodwork to rule out alternative causes.
A diagnosis of exclusion is made if other causes of orthostatic tachycardia, such as blood loss or dehydration, are eliminated.
In my case, medical professionals misdiagnosed the cause of my symptoms for years. Before a knowledgeable doctor saw me and determined the cause, I was told that I had anxiety or a panic disorder and then severe dehydration.
What causes POTS?
Although there is no known cause for POTS, many patients first experience episodes following the onset of a viral infection, a hospital stay, or trauma. For some people, these symptoms may also appear more gradually.
According to Adam Saltman, MD, PhD, the chief medical officer of Eko, "Many causes for POTS have been proposed, from simple dehydration to excessive sympathetic nerve stimulation, deconditioning, and autoimmune dysfunction." However, there is not a lot of concrete evidence to back up any of them.
For years, starting in my 20s, I experienced frequent fainting episodes and unexpected drops in blood pressure. But they became chronic after getting COVID-19 last year. (Johns Hopkins Medicine researchers think the virus can cause POTS. A Johns Hopkins physician established the POTS programme to further investigate the connection and treat the syndrome because enough patients were exhibiting it.)
Conclusion:
Fortunately, treatment works for almost 90% of POTS patients. There is no evidence that POTS shortens life expectancy, nor is it a life-threatening condition.
Additional resources and citations
- 1autonomic nervous system
- 2Parkinson's disease