DENTAL CARE

36 Baby Labour room equipment and their Uses
Baby Labour room equipment are also known as Infant Trays, Baby Trays Surgicals and Baby Delivery Trays. Baby Trays are used in Labor and Delivery room for Baby Receiving.…
WELLNESS HEALTH

The Smart Way to Recover from a Car Accident
Being involved in a car accident can lead to injuries that keep you laid up in a hospital bed or stuck at home for weeks or even months. That recovery…
FITNESS
The Science Behind Resistance Bands: How They Work and Why They're Effective
In recent years, resistance bands have surged in popularity, becoming a staple for athletes, fitness enthusiasts, and even physical therapists. Their versatility and convenience make them a favorite for both…
WHY YOU SHOULD NOT LEAVE YOUR E-BIKE IN THE SUN
Especially in summer, nice weather invites you to go out on your e-bike. However, you should not leave your bike in the sun for too long during a break because…
Home appliances
GE Window Air Conditioner Troubleshooting
GE window air conditioners, like the AEE08AT model, offer excellent options for effectively cooling spacious areas, even large rooms and extra-large spaces, on sweltering summer days. Obstructed filters, power-related concerns,…
HEALTH CALCULATORS
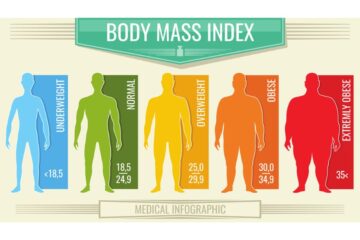
BMI Calculation: Spatz Benefits
Updated:By Isreal Olabanji DST RN0
When discussing weight loss and health, understanding your Body Mass Index (BMI) is crucial. The simple act to calculate your BMI can be a transformative first step. And while there are several methods to tackle weight-related issues, one unique solution stands out:…
pets

Tofu Cat Litter Petsmart
Updated:By Wisdom Bassey0
Tofu cat litter is a type of cat litter made from natural tofu materials. It's typically biodegradable and environmentally friendly, often marketed as a sustainable alternative to traditional clay or silica-based cat litters.…
EDUCATION
Nigerian FG Student Loan Scheme | How to Apply and Secure the Loan
Updated:By Odudu Abasi0
Pursuing higher education can be a significant financial burden for many Nigerian students. To alleviate this challenge, the Nigerian government has introduced the Nigerian FG Student Loan Scheme. This initiative aims to provide financial assistance to deserving students, ensuring that financial constraints…
Skincare

Voghion skincare products benefits
Voghion Voghion provides amazing deals and covers a wide range of popular goods, especially fashion apparel to home, beauty, accessories, shoes and pets. Voghion is an online shopping platform based in London, catering…
Natural Remedies

Home remedy for weight loss
Updated:By Wisdom Bassey0
Weight loss programmes totally exclude carbs and lipids from each meal. Limiting certain nutrients is important, but eliminating them entirely might impair your body's natural processes and metabolism. People attempt various diets every day in an effort to maintain their optimum body…
Tragedy Stories

Trauma in the Digital Age: Social Media, Cyberbullying, and Their Psychological Impact
Updated:By Isreal Olabanji DST RN0
In an era dominated by digital platforms, the internet has become a double-edged sword, offering vast opportunities for learning, connection, and entertainment, but also presenting significant challenges to mental health. The digital age,…
uNDERWEAR

The History of Denims & Trend Evolution Over the Years
Let's talk about a universal style puzzle we've all faced: finding that one wardrobe piece that's effortlessly cool, suits every occasion, and ages like fine wine. Well, here's the secret…

Cotton Panties: A Better Choice than Everyday Options
The comfort level of cotton panties for ladies can vary depending on personal preferences and individual body types. It offers a wide range of products, including clothing, electronics, accessories, and…

WAMA Hemp Underwear Review
Nella has always judged men based on their appearance. And when I mean appearance, I mean from the shirts to their trousers and even their boxer briefs. Crazy right? She…


