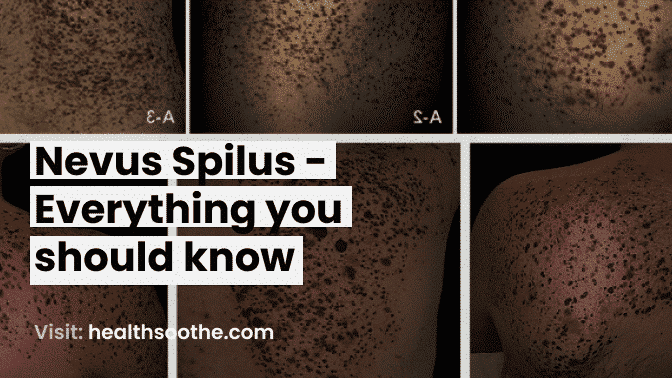
In the hyperpigmented backdrop, the nevus spilus is a well-circumscribed tan macule or patch with several smaller dark brown macules or papules distributed throughout.
About 2-3% of adult Caucasians have one or more of these diseases, which are often acquired during infancy or childhood. Locations on the trunk and extremities are typical.
what is Nevus spilus
A nevus spilus does not go away over time, and exposure to UV light may cause it to become more specked. In these lesions, malignant melanoma and/or atypical nevi are very uncommon. The distribution of larger variants may sometimes be segmental or zosteriform.
Multiple pigmented macules or papules inside a pigmented patch define the cutaneous lesion known as nevus spilus (NS), also known as speckled lentiginous nevus (SLN). Although its cause is yet unclear, it can be congenital or acquired.
Nevus spilus is a skin lesion that affects 0.2% to 2.3% of the general population. Nevus spilus lesions may appear at birth (congenital), develop in youth, or even appear beyond the age of 20. They affect males and women almost equally, as well as individuals of various ethnicities.
Despite instances of melanoma developing inside nevus spilus, the nevus spilus's capacity for malignancy is yet unknown 10. Nevus spilus was formerly thought to be a benign pigmented lesion. However, Perkinson 11 reported the first instance of melanoma developing on nevus spilus in 1957. Less than 40 instances of melanoma emerging inside this organism since then have been documented, some of which have had deadly outcomes.
According to a review of the published literature, Caucasian or black patients accounted for the majority of instances of malignant transformation, which were more often detected on the trunk (64%) than the limbs (36%), had a female-to-male ratio of 56:44, and had an average age of 49 years.
In three earlier occurrences, numerous melanomas were found inside the same nevus spilus, despite melanomas on nevus spilus typically being one tumour.
The most frequent kind of melanomas were superficial spreading melanomas (68%), nodular melanomas (16%), and melanomas in situ (16%). Melanoma is often formed on a small or medium-sized nevus spilus, a zosteriform nevus spilus, or a large nevus spilus in 60% of cases, 24% of instances, or both.
Nevus spilus was present at birth in 52% of patients, acquired during infancy in 33%, and manifested later in 14% of cases 13.
Although the exact risk for malignant transformation in nevus spilus is unclear 14, it is estimated to be between 0.13% and 0.2% 3. When the nevus spilus is macular in type, greater than 4 cm, congenital or acquired in infancy, there seems to be an elevated risk (especially giant and zosteriform variants).
When melanoma first appears, its prognosis and treatment are comparable to those of other melanomas 12. To sum up. Further research is needed on nevus spilus in order to better understand its biological behaviour and pave the way for the creation of uniform management recommendations in the future.
Nevus spilus symptoms
Clinically, nevus spilus often consists of a single, non-hairy lesion that is 4.3 cm ( 3.5 cm) in size on average. Macular rather than papular spotting, measuring 1-3 mm, often develops over months to years inside the lesion.
Nevus spilus may be broken down into macular and papular variations as well as into three size categories: tiny (1.5 cm and less), medium (1.5 to 19.9 cm, and large (>20 cm). Segmental/zosteriform nevus spilus has also been reported, albeit it is less common. Anywhere on the body might develop lesions, but the trunk and extremities are most susceptible.
Nevus spilus diagnosis
The clinical appearance is often used to make the diagnosis of nevus spilus. If there is any uncertainty, a dermoscopy or a biopsy sample taken from the lesion for histology may reveal distinctive microscopic characteristics.
Nevus spilus treatment
Nevus spilus does not have a consistent management strategy. In conclusion, patients should be instructed to self-examine their nevi to check for any changes and get a systematic long-term follow-up using sequential digital dermatoscopy and, if possible, reflectance confocal microscopy.
This method, together with the prudent use of biopsy for worrisome spots, seems to help in the early diagnosis of melanoma. The existing research does not support the removal of nevus spilus as a preventative measure without pathologic verification of dysplasia or cancer.
NS has spawned a number of management strategies. There have been both aggressive and cautious therapeutic methods used.
Excision is necessary in cases of melanoma transformation. In these circumstances, the whole NS must be removed in order to stop recurrence and remove the field defect; this may leave a significant scar.
Complete nevus spilus excision is appropriate, size allowing, in cases of dysplasia or malignant melanoma in order to remove the "faulty backdrop" and seek for any multifocal melanomas.
Is nevus spilus benign?
Nevus spilus is a benign lesion, hence there is no need for treatment. Malignant melanoma may develop in nevus spilus, however, this is an uncommon occurrence and the risk is the same as for melanoma to develop in an acquired or congenital nevus.
Multiple pigmented macules or papules inside a pigmented patch define the cutaneous lesion known as nevus spilus (NS), also known as speckled lentiginous nevus (SLN). Although its cause is yet unclear, it can be congenital or acquired.
Conclusion:
For NS, there isn't a set management strategy. In conclusion, patients should be instructed to self-examine their nevi to check for any changes and get a systematic long-term follow-up using sequential digital dermatoscopy and, if possible, reflectance confocal microscopy. This method, together with the prudent use of biopsy for worrisome spots, seems to help in the early diagnosis of melanoma.
The research that is currently available does not support prophylactic NS removal without pathologic confirmation of dysplasia or cancer. Complete NS excision is appropriate, size allowing, in cases of dysplasia or malignant melanoma in order to remove the "faulty backdrop" and look for possible multifocal melanomas.
In order to better understand NS's biological behaviour and enable the creation of uniform management recommendations in the future, further research is necessary. As far as we can tell.