‘Pelvic Organ Prolapse is ruining my life!’ – This is the mantra of nearly one-third of women of all ages, especially moms.
If you are experiencing pelvic organ prolapse, you are not alone. Nearly one-third of women of all ages experience this condition at some point in their lives. While not usually a major health issue, the condition can potentially be uncomfortable, embarrassing, and hinder your quality of life.
There is no need to suffer in silence. A variety of simple solutions and enhanced treatments can help. Learn about the causes of pelvic organ prolapse and what you can do to help relieve the symptoms.
This article shows some experiences of past and present pelvic organ prolapse sufferers, how the prolapse affected them, and how they coped with it to become hale and hearty again.
My article also covers how pelvic organ prolapse can ruin your life, and what to do to recover from any damage the prolapse caused.
What Exactly Is Pelvic Organ Prolapse (POP)?
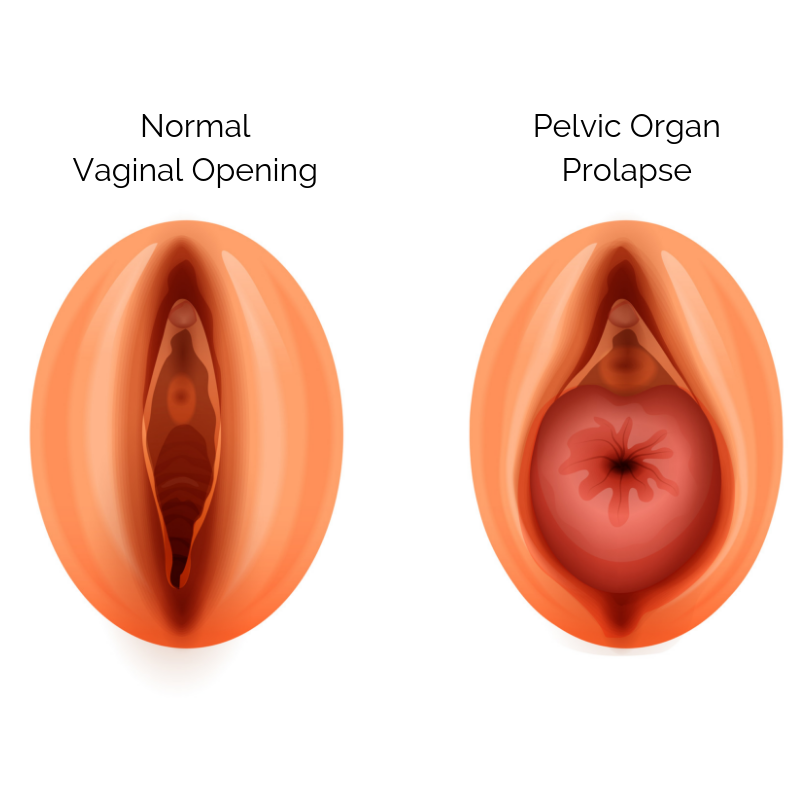
In the bottom of your pelvis are your pelvic floor muscles and tissues. They act like a hammock or a trampoline supporting your pelvic organs (like your bladder, uterus, and rectum).
A prolapse happens when these muscles and tissues get damaged or become incredibly weak and can’t properly support one or more of your pelvic organs. Once that support is compromised the organs fall down farther in the pelvis than they’re supposed to sit.
There are a few different issues and events that can cause prolapse. Like a long, hard pushing phase during labor, the use of instruments during labor (forceps or vacuum), the drop in estrogen during menopause that can weaken pelvic floor tissues, and chronic lung diseases (like asthma) that cause you to cough a ton, to name a few.
Whatever caused the prolapse? It’s important to know that this is not your fault. It isn’t. You have enough guilt in your life, you don’t need to add “I did (or didn’t) do something, and now I have a prolapse” to the list.
The best thing you can do is get help as early as possible. You want the best chance of getting as much function back to the muscles and tissues as possible. But it’s never too late and there are plenty of options to help your pelvic organs out – regardless of how long ago you had your baby.
There are a few different types of prolapses.
The 3 most common prolapses are:
- Bladder (Cystocele)
- Uterus (Uterine)
- Rectum (Rectocele)
If you have one of these types, it simply means that your bladder, uterus, or rectum is drooping down instead of staying perched up where it’s meant to be.
It’s also possible to have more than one prolapsed organ. Both your bladder and uterus could be prolapsed, for example.
There are also different grades or classifications of prolapse:
For now, here’s the basic outline:
- Grade 0 (no prolapse)
- Grade 1 (the organ or organs are slightly drooping down, while still being more than 1 cm above the level of the hymen)
- Grade 2 (the organ or organs have come down a bit further and are 1 cm or less above the level of the hymen)
- Grade 3 (the organ or organs have slid pretty far down and are now more than 1 cm below the level of the hymen)
- Grade 4 (the organ is causing your vaginal wall to bulge out of your vaginal opening)
With every sentence I type (Grade 4, I’m looking at you) I feel compelled to write “It’s okay! Please don’t stress! There’s hope!”
I know this can feel overwhelming and the opposite of fun but stick with me. No matter how mild or severe your symptoms are, there’s absolutely hope. There always is. And the truth is that symptoms vary and no two cases are the same.
Some women have a grade 3 or 4 prolapse with very little to no symptoms. Others have a grade 1 or 2 prolapse with significant symptoms.
This is why it’s important that you focus less on the classification and more on your unique symptoms. And remember that regardless of what’s going on for you, there are options and strategies that can help.
Signs You Could Have It
It’s estimated that around 50% of women have some degree of prolapse after giving birth. But only 10-20% of women report symptoms of prolapse.
This means that most women with prolapse don’t actually have symptoms. It’s not severe and as long as they take steps to support their core and pelvic floor recovery postpartum – which I recommend all women do – they likely will continue to be asymptomatic throughout their life.
The truth is that our pelvic organs don’t need to stay in the exact same place our entire lives. They’ll likely shift during pregnancies and postpartum, throughout our menstrual cycle, and during menopause.
This is normal. The key is to simply be aware and mindful of any symptoms you may have without obsessing over them (which can be easier said than done if you’re Googling all the things worrying that you have prolapse and wondering how to fix it).
And take the appropriate steps to ease your symptoms if they do come up. If you do have symptoms, they may look something like this:
- Heavy feeling in your vagina
- Feeling like you need to pee but it won’t all come out
- Lump or bulge in your vagina or vaginal opening
- Feeling like something is falling down or dropping when you cough, sneeze or jump
- When you sit it feels like you’re sitting on something – like a small ball or an egg
- Issues with leaking
- Having problems pooping (constipation) or feeling like you can’t fully empty your bowels
- Painful sex
- Not feeling much, or having less sensation when you do have sex
- Back pain that gets better when you lie down
- Abdominal pain
- Having trouble keeping a tampon in
- Getting bladder infections a lot
Remember – you can get all or just some of these symptoms.
Pelvic Floor Prolapse is Ruining My Life! – How Can This Prolapse Do This?
I will be dropping an experience someone had with POP which will show how it can put you in a bad place and to further attest to this statement: ‘prolapse are ruining my life’.
Read Carolyn’s story:
I’ve dealt with recurring bladder and urinary tract infections since at least my college days. I would always go to doctors to take care of it, but the conditions kept coming back.
What I didn’t know until much later was that I had a weak pelvic area, and going through three pregnancies over the years probably made the situation worse.
By the time I came to UT Southwestern, I felt like life as I knew it was over. This is going to sound pretty graphic, but when your pelvic floor prolapses, or drops, it feels like a baseball is trying to work its way out of your posterior, and then that same pressure will transfer to the vaginal area. It’s horrible.
I began to not go anywhere. I began to tell people, “No, I can’t go out to eat,” “No, I’m just going to stay home.” And then I’d take something for the pain, but nothing really helped. The only comfortable position at the worst of times was lying flat.
I love to scuba dive, but I even began to stay away from that because I was concerned about putting that tank on my back. I stopped going for walks. Worst of all was not being able to pick up my grandchildren – because any time you pick up something, the pressure goes right to the pelvis.
Even sitting for long stretches became unendurable, which was a major problem because my grown children live in D.C. and L.A., and sitting in an airplane for that long made the “baseball butt” feeling just unbearable.
So, it really was a miserable time, because who do you talk to about that? You don’t want to tell anybody, and, consequently, you just sort of live in shame.
Eventually, I did tell some of my friends what I was going through, and once that happened I began to hear of so many women who were going through exactly or something like the very same thing.
Fortunately for me, I’d become familiar with UT Southwestern several years earlier when doctors there treated my daughter for an entirely different condition. Those doctors became like family, and through them, I got referred to see Dr. Philippe Zimmern.
When I described to him what I was going through, he immediately knew what to do and set everything in motion. And, just as immediately, life started changing.
Dr. Zimmern performed my bladder suspension surgery, which is a procedure that restores the bladder to its normal position, and that was followed by pelvic floor physical therapy with Dr. Kelly Scott. I can’t even describe how much of a life-changer that was. I drove to UT Southwestern in Dallas from my home in Waco for 19 consecutive Mondays that year just because that physical therapy with Dr. Scott and my PTs, Michelle Bradley, and Jenn Huneidi, were so amazing. Soon I was back to walking and working out and doing everything in my life I had thought was over.
Now, at 60 years old, I can tour D.C. and traipse up and down the beach in L.A. – and I do!
Meanwhile, I’ve fulfilled a goal I’ve had for 30 years by going back to school. On May 16, I completed a two-year master’s program in social work – which involved a 25-hour-per-week internship and carrying 12 to 13 hours per week of homework, on top of my regular job. I could have never done that prior to my pelvic floor disorder treatment.
I really feel I owe UT Southwestern for giving me my life back – specifically Dr. Zimmern and Dr. Scott but so many others there as well. It was truly a team effort, and, from top to bottom, it was one of the most dignified, compassionate, and best-practice teams I’ve ever witnessed.
My message to the many, many women who are going through what I did – or anything like it – is that you don’t have to endure it. Find someone to talk to and describe your symptoms. You are definitely not alone, and there is a way to get back your quality of life, which is so important.
There can be a lot of fear and confusion and overwhelm around the idea of a prolapse. Most of that stems from the fact that hardly anyone talks honestly about it in a practical way (beyond “Don’t lift heavy weights”), and the internet is full of horror stories.
The truth is that prolapse is scary when you don’t completely understand what you’re dealing with and you don’t know how to “fix” things. You might feel less confident about having sex, doing certain exercises, or getting pregnant with another baby because you’re afraid it’ll make things worse.
But there are pros and tools and strategies you can use to help get your life back. The next section shows what I recommend you do.
Watch the video below to see the impacts of POP, and further more understand why people say 'pelvic organ prolapse is ruining my life'.
Prolapse Is Ruining My Life - Living Your Life to The Fullest with Pelvic Organ Prolapse
Here’s what I recommend you do on to cope with a POP instead of just saying ‘prolapse is ruining my life’:
Step 1: Book an appointment with a pelvic health physio
This is a critical first step because a pelvic floor physiotherapist or physical therapist can do an internal assessment to see what exactly is going on in there and give you the next best steps for your body.
No two cases of POP are the same so we want you to get what you specifically need.
Some pros will also get you to stand up, and maybe even do some gentle exercises, and do an assessment while you’re standing or doing certain movements. I think this is a fantastic idea because sometimes when we’re laying down it’s hard to tell exactly what’s going on. But once we’re standing and moving, it’s easier to get the whole picture.
Remember – you are in charge of your own health so find a great, qualified pro to help you out. If you aren’t happy with the experience you’re getting, find someone else.
This is your body. Your life. You don’t have to just live with the discomfort and worry. Find someone who supports your goals and is willing to do whatever they can to help make that happen.
Step 2: Pay attention to what exercises and events bring on symptoms
Does running make you feel heaviness in your vagina? If you’re on your feet all day do you feel like you can’t control your bladder by 7 pm? When you do that deadlift with that weight does it feel like something is bulging out of your vagina?
Do your symptoms get worse when you’re ovulating or menstruating? When you’re tired or stressed, do your symptoms creep up more?
Paying attention to what’s going on in your body as you go about your day and your workout is crucial to better understand the steps you can take to help feel stronger.
It may simply be a matter of trying different exercises, different variations of an exercise, doing fewer reps, taking more rest, or starting out with less weight and then progressively challenging your body in a way that makes it feel like it can handle the pressure.
It may also help to adjust your training around your cycle (which can be helpful for all women – not just women with prolapse). If you know that you get more symptomatic when you’re ovulating, that can help inform the type of exercise you do during that period.
And of course, you’ll also want to work on your breathing techniques, getting in better alignment, and engaging your core to support your pelvic organs (instead of generating more downward pressure into your pelvic floor). You don’t have to stop doing the exercises you love forever.
But if you’re getting symptoms when you do that particular exercise, with that particular weight, in that particular way, we need to troubleshoot and figure out what’s going on so we can get you to a place where your symptoms are no longer an issue every time you try to work out.
Step 3: Release & relax and also build up your pelvic floor strength
It’s pretty obvious that if your pelvic floor is compromised, working on strengthening it will likely help alleviate some (and maybe even all) of your symptoms. But what you may be surprised to hear is that releasing and relaxing your pelvic floor is key too.
In fact, many women discover that a tight pelvic floor is actually creating more symptoms for them. Yes. A too-tight pelvic floor can actually make your prolapse symptoms worse.
This can be especially true if you’re under a lot of stress. When we’re stressed, we have a tendency to tense up. Think of how tight your shoulders can get after a hard week with a teething baby and work deadlines galore!
Now imagine what your pelvic floor is doing. Right? That’s why doing some pelvic floor-specific relaxation and meditation exercises can be really effective.
You can do a mobility flow like the video below to help release the tension, and you can also spend 2 minutes in meditation using a progressive relaxation technique.
For progressive relaxation, lay down on the floor, close your eyes, and take a deep breath in, then exhale as you tighten your pelvic floor muscles (do a kegel), then inhale and release and relax all the muscles in your pelvic floor and your bum. Do this 3 – 5 times.
These techniques can be especially helpful when you’re getting more symptoms than usual.
We also want to focus on strengthening your pelvic floor. This doesn’t necessarily mean that 5 sets of 10 kegels daily are what you need. It may be the case. But not always.
Rehab can look like kegels and clamshells. Or it may be squats and rows. It really depends. And the truth is that there really isn’t a set of “prolapse healing” exercises that you can do because it’s not just about what exercises you do, it’s also about how you do them.
So (at the risk of sounding like the world’s most broken record) pay attention to your breathing, your alignment, and your technique. And be curious about how your body feels during and after a certain workout or exercise.
Check in with your postpartum fitness pro, physio, midwife, or doctor to see what the best options are for you.
And if you are exercising – especially in those early months of playing around with exercising with prolapse – remember to exhale and engage your core and pelvic floor as you do the most challenging part of the exercise. I call this the BED Mantra. It can help your pelvic floor better support your organs during your workout.
Step 4: Explore the idea of a pessary
If you want to run, lift heavy, jump rope, and generally be more active but you’re worried those things can (or already are) making your prolapse symptoms worse, or you simply want some relief from the symptoms you’re getting in your daily life, you can look into getting a pessary.
A pessary is a small silicone device that can be made in many shapes and sizes. You put it in your vagina as a space occupier or to help support your pelvic organs. You can think of it like a sports bra for your pelvic organs. Don’t worry, you won’t even be able to feel a properly fitted pessary.
For some women, a pessary not only helps them feel physically able to do the workouts they want to be doing, but it also helps them relax mentally. Having the extra support can help them ditch some worries about making things worse.
So if you find yourself clenching your vagina (consciously or unconsciously) during your workouts (or all day, every day) because you’re worried about making your prolapse worse, a pessary could be your new bestie.
If you’re curious, this is something you can chat about with your physical therapist, physiotherapist, or doctor. The best news? A study of 106 women with stage 2 or greater POP showed that most women saw a significant improvement in POP symptoms when they used a pessary. So a pessary can work incredibly well if you find the right choice for you.
A quick tip: I have heard some doctors say that young moms don’t need pessaries. That they’re only for older ladies. This is absolutely untrue. Why wait when you can improve your quality of life now?
So if you get some pushback, find a healthcare provider who is more supportive of what you’re going through and the options that can help.
And remember that it may take a bit of effort to get the right fit. Some research shows that, “On average, 2 to 3 fittings were required until the appropriate pessary was found.” So if it’s not fitting right, don’t be afraid to go back and get re-fitted. You deserve to feel good and this means getting a pessary that fits well.
What if I’ve Done All the Treatments Available and Yet Still, Prolapse is Ruining My Life?
If you’ve worked with a pro to rehab your pelvic floor, your alignment, engagement, and breathing strategies are on-point, you’re getting some relaxation and release sessions in, and you’ve tried a pessary, but you’re still getting symptoms and you feel like you need something else to help, then surgery may be a great option for you.
This is something you’d want to consult with a urogynecologist or other pro about (different pros may take on this role depending on where you live).
Just remember that surgery is typically best for women who have already tried rehabbing their pelvic floor and have tried other strategies and options so that the chances of successful surgery are improved.
You can think of pelvic floor rehab as prep work for surgery because you’ll know how to properly support your pelvic organs post-surgery and boost your chances of having the results you’re wishing for.
Surgery is an option. It just doesn’t have to be the only option and usually isn’t the first step you’d take. The bottom line is that it’s your body, your choice. Do what feels best for you.
There’s Always Hope
Growing and birthing tiny humans is not an easy task. Add to that the potential for issues like prolapse and you can end up feeling depressed, alone, and wondering if you’ll ever feel like yourself again. But it doesn’t have to be that way.
I hope that this post gave you some tools and strategies you feel confident running with (maybe even literally!) Because there’s always hope. Prolapse can be a scary, overwhelming, “I have so many questions” thing. But it doesn’t have to be.
You now have a better idea of who to turn to for support and the tools you need to feel stronger and more confident. Use ’em. There’s no such thing as 10 Quick Steps to Healing Prolapse but you don’t need them.
Take the right small actions every day and you will see progress. It may be slow. It may look more like an up-and-down squiggle and less like a straight line. But it will still progress.
You’ve got this and You deserve this.
Many women with prolapse don't need treatment, as the problem doesn't seriously interfere with their normal activities. Lifestyle changes such as weight loss and pelvic floor exercises are usually recommended in mild cases. Pelvic organ prolapse doesn't necessarily get worse over time, and you may not need treatment if the symptoms are not affecting your daily life. Nonsurgical treatments for pelvic organ prolapse can reduce the pain and pressure of mild-to-moderate prolapse and preserve fertility if the uterus is prolapsed. Protect your prolapse from worsening during everyday activities by: Prolapse is also associated with repetitive heavy lifting, chronic constipation, chronic cough, and weak or poor tissue. Prolapse symptoms may be worse at different times in the day. Some women notice that they feel more pressure after walking or standing for long periods of time. Symptoms of moderate to severe uterine prolapse include:Frequently Asked Questions About Pelvic Organ Prolapse (POP)
Can you live a normal life with a prolapse?
Can you live with a prolapse without surgery?
How can I be comfortable with a prolapse?
Why is my prolapse getting worse?
How do you know if your prolapse is severe?