Pericoronitis is an inflammatory condition that commonly affects the lower mandible when there is a partial eruption in the soft tissues surrounding the tooth. It sets in when there is an accumulation of food that remains under the operculitis and a bacterial infection arises from it. It can be chronic or acute and give off symptoms of varying seriousness.
Pericoronitis is one of the many dental conditions that affect humans, regardless of gender. It can also occur when you have bitten down on the operculitis – covering the partially emerged tooth – with the opposing tooth.
In this article, you will understand pericoronitis; its causes, symptoms, and treatment. Specifically, we will delve into how you can treat this dental issue at home and tips for self-care when you have pericoronitis.
What is Pericoronitis?

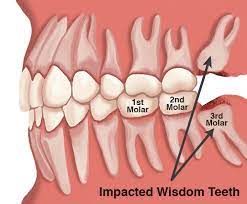
The third molar, also called wisdom tooth is the primary reason there is a condition called pericoronitis. This last molar that usually grows later in life – between the age of 17 and 21 – causes some pain when it grows. Normally, it shouldn’t but when it does, it is usually due to pericoronitis, which may be brought on as a result of a bacterial infection or a mechanical trauma such as biting down hard on it.
Pericoronitis is a dental condition that is characterized by the inflammation of gum tissue – operculitis – that partially covers the tooth’s crown since it has not fully emerged. Pericoronitis occurs as a result of the inadequate space for the just emerging molar to receive oral hygiene.
It is classified into chronic and acute, which says nothing about the cause of the inflammation but the severity of the symptoms. Although pericoronitis typically occurs when the wisdom tooth is emerging, which is during the teenage and early adult years, it can also occur in teething kids.
Chronic pericoronitis usually happens with subtle or no symptoms and as it is in their nature to be recurrent, the symptoms may, sometimes, be acute. However, acute pericoronitis is short-lived and may present some serious symptoms like fever or swollen lymph nodes around the neck.
Causes of Pericoronitis
Since it is difficult to reach the crown of the tooth at the end of the mandible – especially because it is emerging and the crown is not fully visible, yet – It is difficult to properly clean the crown and rid it of food remains and particles.
Most times, these food particles hide under the tissue that covers the crown and when they remain there, bacteria grow on them, leading to pain and sometimes they can become abscessed, which is filled with pus.
Also, pericoronitis can be caused by mechanical disturbance of the tissue covering the tooth’s crown. In this case, it is possible that the operculitis get bitten down on, hard, or they might get hit by a toothbrush during oral hygiene practice.
Symptoms of Pericoronitis
Regardless of whether the classification of pericoronitis is chronic or acute, when they come with symptoms, they are usually one or more of these ones listed here. The severity of these symptoms is what signifies if your pericoronitis is acute or chronic.
- Ache in the affected area for a couple of days
- Bad breath (Halitosis)
- Unusual taste in the mouth
- Pus under the tissue covering the crown
- Inflamed gum tissue
- Difficulty swallowing due to pain
- Trismus
- Severe back teeth pain
Some of these symptoms, such as ache, might be severe if your pericoronitis is acute.
Treatment of Pericoronitis
Pericoronitis can be caused by different factors. However, its treatment is usually straightforward:
- Alleviate the pain
- Remove the flap, or
- Remove the tooth.
Your doctor will recommend that you undergo one or more of these treatment options, depending on the seriousness of your pericoronitis. Usually,
- Your doctor will recommend you manage the pain that comes with pericoronitis regardless if it is classified as acute or chronic. Pain killers such as aspirin and paracetamols will effectively help to assuage the pain.
- The first surgical option of treatment is to remove the tissue that covers the tooth crown. The flap is removed and the patient is fine. However, in some cases, the flap grows back and a second surgery is required.
- The final treatment option, when all other treatment options are ineffective, is to completely remove the tooth. In this case, other treatment options are done before this.
Generally, it is usually effective to alleviate the pain, clean the surrounding of the inflamed tissue, and use antibiotics, if there is an abscess.
Home Treatment and Self-care for Pericoronitis
While getting professional treatment should not take a back seat when it comes to your health, it is advisable that you combine the professional health care you are given with some treatments you can give yourself at home, at the approval of your dentist or oral surgeon, that is.
Some of the home treatment you can use to help yourself with pericoronitis are:
Rinse your mouth with warm water and salt mixture
A warm salt-water mixture will help to disrupt the colony of bacteria that may be growing under the gum tissue flap and in the long run, reduce the severity of the symptoms.
Practice good oral hygiene consistently
The secret to perfect oral health is to consistently practice good oral hygiene. Brush your teeth, with good technique, at least twice daily, floss your teeth to remove food particles hanging in spaces and crevices, rinse your mouth regularly to avoid plaque development.
Use over-the-counter analgesics
To deal with the pain that comes with pericoronitis, buy some over-the-counter pain killers and use them. Ibuprofen and Tylenol are available for sale in many pharmacies and they will help you bring the pain down.
Use oral irrigators
Irrigate the inflamed site of your gum to help you deal with the pain and disrupt the bacterial colony that may be there. Oral irrigators help you to apply a water-salt mixture or any other effective mixture directly to the inflamed site. Here are the full remedies Pericoronitis Home Treatment: 12 Home Treatment For Pericoronitis Pain And Discomfort
Conclusion
Pericoronitis is a dental condition that is associated with the growth of the last set of teeth (molars) and it is characterized by pain that develops as a result of bacterial infection under the gum tissue flap that covers the crown of the emerging tooth.
It is majorly caused by mechanical trauma or bacterial infection to the growing tooth. This is possible when an individual does not practise effective oral hygiene to remove food particles from underneath the tissue flap; it can be difficult to achieve.
However, it can be treated by administering pain killers or surgery that removes the flap or the tooth.
REFERENCES:
Hazza'a A. M., et al. "Angulation of mandibular third molars as a predictive factor for pericoronitis." The Journal of Contemporary Dental Practice 10.3 (2009): 51-58.
Nguyen, D., et al. "Common Dental Infections in the Primary Care Setting." American Family Physician 77.6 (2008): 797-802.
Medicine net, pericoronitis centre
https://www.medicinenet.com/pericoronitis/index.htm
College of Medicine, University of Ibadan, Nigeria, and others
http://uch-ibadan.org.ng
https://com.ui.edu.ng/index.php/en/

Isreal olabanji a dental assistant and public health professionals and has years of experience in assisting the dentist with all sorts of dental issues.
We regularly post timely and trustworthy medical information and news on Fitness, Dental care, Recipes, Child health, obstetrics, and more.
The content is intended to augment, not replace, information provided by your clinician. It is not intended nor implied to be a substitute for professional medical advice. Reading this information does not create or replace a doctor-patient relationship or consultation. If required, please contact your doctor or other health care provider to assist you to interpret any of this information, or in applying the information to your individual needs.