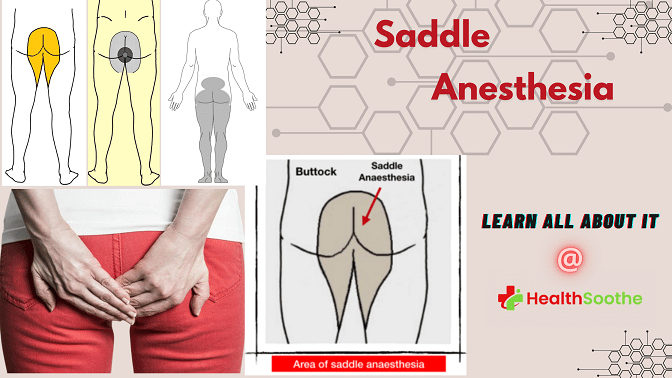
Have you ever had the loss of feeling or sensation loss at the area of your buttocks, the inside parts of your thighs, and your waist area (perineum), and wondered what it is, what causes it, and how you can treat it?
Quick Facts About Saddle Anesthesia
| A | B |
|---|---|
| Meaning | Saddle Anesthesia is a loss of sensation experienced in the areas that would touch a saddle when riding a horse – the buttocks, perineum (external genitalia and anus), and inner thighs |
| Causes | It can be caused by nerve compression or injury in the lower spine, such as the sacral nerves, due to herniated discs, spinal stenosis, trauma, tumors, spondylolisthesis, or other factors like aging, injury, or repetitive movements |
| Symptoms | Symptoms include lack of sensation, tingling, or partial feeling in the affected areas |
| Related Conditions | Frequently associated with cauda equina syndrome and may also relate to conus medullaris syndrome |
| Diagnosis | Clinical examination by a healthcare provider, possibly followed by imaging tests like MRI or CT scans to identify the underlying cause |
| Treatment | Treatment focuses on addressing the underlying cause, which may involve medication, physical therapy, physical therapy, pain management, steroid injections, or surgery in severe cases |
| Prevention | Preventive measures include maintaining proper posture, avoiding repetitive stress, and seeking early treatment for back injuries |
| Complications | Loss of bladder or bowel control, sexual dysfunction, and mobility issues may occur if not promptly addressed |
| Prognosis | Varies based on the cause and severity; early diagnosis and appropriate treatment can often improve symptoms and prevent complications |
This sensation loss could be saddle anesthesia. Yeah, you read right. I said that sensation loss you are experiencing from your waist region to your thighs could be saddle anesthesia. Have you ever heard about it? What of saddle anesthesia block1wikipedia Pudendal_anesthesia? - Have you heard of it as well?
Well, if you haven’t, or if you have, and you still want to know more about it, then you are in the right place.
Today’s article from Healthsoothe will explain all there is to know about saddle anesthesia - its causes, symptoms, complications, diagnosis, and treatments, as well as how to prevent it from ever happening if you don’t have it already.
Alright, what are we waiting for? Let’s proceed!
Saddle Anesthesia – What is it?

Saddle anesthesia is a sensory loss (anesthesia) that is limited to the buttocks, perineum and inside borders of the thighs.
Asymmetric saddle anesthesia is frequently associated with the spine-related injury cauda equina syndrome2"Cauda Equina Syndrome". Retrieved 2022-10-02.. It is also seen symmetrically with conus medullaris and may occur as a temporary side effect of a sacral extradural injection3Gerald L Burke, MD. "Backache from Occiput to Coccyx". Retrieved 2022-10-02.. Saddle anesthesia also may develop during anorectal surgery with intrathecal fentanyl 15 g.
Saddle Anesthesia, Cauda Equina Syndrome, and Conus medullaris syndrome – How is each related?
We have already established that cauda equina syndrome, a spine-related injury, is usually linked with asymmetric saddle anesthesia. This means that saddle anesthesia is closely linked to cauda equina syndrome, and one rarely happens without the other. And conus medullaris syndrome is also linked to saddle anesthesia.
So, if a person is diagnosed with cauda equina syndrome or conus medullaris syndrome, or even both, then there is a high possibility that the person also has saddle anesthesia.
This goes further to say that the symptoms, causes, diagnosis, and treatments, along with the prevention of conus medullaris syndrome and cauda equina syndrome are related to that of the saddle anesthesia.
Cauda equina syndrome is a life-threatening emergency caused by disruption and compression of the operation of these nerves. It may include or be distal to the conus medullaris and most often happens when the L3-L5 nerve roots are damaged.
Back discomfort spreading to the legs, sensory and motor impairment of the extremities (lower), bladder or dysfunction of the bowel, sexual dysfunction, and saddle anesthesia are all symptoms of cauda equina syndrome.
Cauda equina syndrome is particularly fraught with litigation since lags in diagnosis and treatment may result in serious life-long damage.
Cauda equina syndrome patients may face varying degrees of the following issues:
- Loss of sensation in the legs
- Loss of feeling in or around the genitals and/or rear passage
- When wiping the anus after defecation or excretion, there is the inability to feel the contact or touch of the toilet paper
- Sensation of tingling in the saddle region
- Weakness in the saddle region
If you suffer saddle anesthesia, contact your doctor or the local emergency center very away. They should be able to determine if you have conus medullaris syndrome or cauda equina syndrome.
Conus medullaris syndrome and cauda equina syndrome are uncommon, with a yearly rate of one in 30,000 to 100,000 persons. Annual incidence estimates range from 1.5 - 3.4 per million individuals.
It affects 3 percent of the total of all disc herniations. Conus medullaris syndrome and cauda equina syndrome are more prevalent in young males, presumably because this demographic is more prone to suffer from compressive thoracolumbar trauma.
According to one research, we might anticipate 449 new cases of conus medullaris and 1016 new instances of cauda equina syndrome in the United States per year.
To know more on how saddle anesthesia is related to conus medullaris and cauda equina syndrome, watch the first video in this article.
What Causes Saddle Anesthesia?

The principal causes of saddle anesthesia are tumors, lumbar spinal stenosis, ruptured lumbar disc, arachnoiditis, and a spinal fracture.
Remember when I said that the symptoms, causes, diagnosis, and treatments, along with the prevention of conus medullaris syndrome and cauda equina syndrome are related to that of the saddle anesthesia.
So, right now, we are going to know what causes saddle anesthesia by knowing what causes the conus medullaris syndrome and cauda equina syndrome. The anatomy and clinical appearance of the conus medullaris and cauda equina syndromes overlap.
The conus medullaris is seen to be the spinal cord's terminal end, which occurs in the average adult just at L1 vertebral level. Conus medullaris syndrome occurs when the spinal cord is compressed from T12-L2.
The cauda equina is a set of nerves and nerve roots that arise from the distal part of the spinal cord, generally levels L1-L5, and include axons of nerves that innervate the bladder, perineum, legs, and anus with both motor and sensory innervation.
Cauda equina syndrome is caused by compression and disturbance of the operation of all these nerves and may include or be distal to the conus medullaris. It most often happens when the L3-L5 nerve roots are damaged.
Both disorders are neurosurgical emergencies because they may cause back pain that radiates to the legs, lower extremity motor and sensory dysfunction, bladder or dysfunction of the bowel, sexual dysfunction, and saddle anesthesia.
Cauda equina syndrome and conus medullaris syndrome are similarly at significant risk of legal action since delays in diagnosis and treatment may result in serious life-long damage.
Pressuring of the spinal cord and nerves/nerve roots emerging from L1-L5 levels causes conus medullaris syndrome and cauda equina syndrome. The herniated lumbar disc is the most prevalent cause of compression in 45% of cases with cauda equina syndrome.
Other reasons include spinal epidural hematoma, malignancy (either metastatic or primary brain and spinal cord cancer), discitis, epidural abscess, trauma (especially if bone fracture pieces are retropelled), aortic blockage, and spinal stenosis.
Cauda equina syndrome has been linked to chiropractic manipulation, and the implantation of interspinous devices, including inferior vena cava thrombosis in rare circumstances.
The Symptoms of Saddle Anesthesia
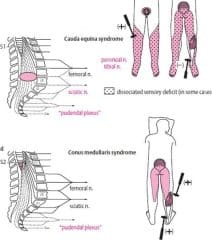
Patients with saddle anesthesia may exhibit symptoms of isolated conus medullaris syndrome, solitary cauda equina syndrome, or a mix of the two.
Cauda equina syndrome symptoms and signs are predominantly lowered motor neuronal in nature, while conus medullaris syndrome symptoms and signs are a mix of upper motor neuron and lower motor neuron effects.
The onset history, length of symptoms, and presence of additional traits or symptoms may all point to plausible reasons.
Symptoms and signs of Conus Medullaris and Cauda Equina Syndromes
| Focus | Cauda Equina Syndrome | Conus Medullaris Syndrome |
| Reflexes | Both ankle and knee jerks affected | Knee jerks preserved but ankle jerks affected |
| Low back pain | Less | More |
| Radicular pain | More severe | Less severe |
| Presentation | Gradual and unilateral | Sudden and bilateral |
| Motor strength | Asymmetric areflexic paraplegia that is more marked; fasciculations rare; atrophy more common | Typically symmetric, hyperreflexic distal paresis of lower limbs that is less marked; fasciculations may be present |
| Sphincter dysfunction | Urinary retention; tends to present late in course of disease | Urinary retention and atonic anal sphincter cause overflow urinary incontinence and fecal incontinence; tend to present early in course of disease |
| Impotence | Less frequent; erectile dysfunction that includes inability to have erection, inability to maintain erection, lack of sensation in pubic area (including glans penis or clitoris), and inability to ejaculate | Frequent |
| Sensory symptoms and signs | Numbness tends to be more localized to saddle area; asymmetrical, may be unilateral; no sensory dissociation; loss of sensation in specific dermatomes in lower extremities with numbness and paresthesia; possible numbness in pubic area, including glans penis or clitoris | Numbness tends to be more localized to perianal area; symmetrical and bilateral; sensory dissociation occurs |
Cauda equina syndrome symptoms include the following:
- Pain in the lower back
- Sciatica may be unilateral or bilateral.
- Hypoesthesia or anesthesia of the saddle and perineum
- Disturbances in the bowel and bladder
- Sensory and motor impairments in the lower extremities
- Lower extremity reflexes that are reduced or missing
Low back pain is classified as either local or radicular. Local pain is characterized by severe, agonizing pain caused by the vertebral body and soft-tissue irritation. Radicular pain is characterized by acute, stabbing pain caused by constriction of the roots of the dorsal nerve.
Radicular discomfort manifests itself in dermatomal distributions. Cauda equina syndrome low back pain may have several characteristics that distinguish it from the considerably more frequent lumbar strain. Patients may describe severity or an unexpected trigger, like head tilting.
Severe pain is seen early in 96% of individuals having the cauda equina syndrome caused by a spinal tumor. Later findings included lower extremity weakness caused by ventral root involvement. Hypotonia and hyporeflexia are common symptoms. Sphincter dysfunction and sensory loss are also frequent.
The following are urinary symptoms of cauda equina syndrome:
- Retention
- Difficulty starting to urinate (micturition)
- Reduced urethral sensation
- Urinary bladder problems often starting with urinary retention and progressing to overflow urinary leakage.
Bell et al revealed that the precision of urine retention, frequency, incontinence, changed urinary sensation, and changed perineal feeling as indicators of potential disk prolapse warranted immediate MRI evaluation.
The following are examples of bowel disturbances:
- Incontinence
- Constipation
- Anal tone and sensory loss
The first sign of bladder or bowel malfunction may be trouble initiating or halting a urine stream. It is possible that it will be accompanied by outright leakage, first of pee, then of feces.
Overflow is the cause of urine leakage. It is generally combined with saddle anesthesia (the physician can ask if toilet paper feels differently when wiping).
Watch the first video in this article, to know more on the signs and symptoms of saddle anesthesia.
The Complications of Saddle Anesthesia
Complications with cauda equina syndrome and conus medullaris syndrome occur in a significant proportion of patients diagnosed. One research looked at 63-day results in cauda equina syndrome for micturition, feces, the saddle anesthesia, sexual performance, and sciatica.
The statistics show that a high number of patients, regardless of the time until surgical decompression, still have lingering symptoms. Micturition deficiencies such as retention necessitating self-catheterization or the presence of indwelling or suprapubic catheters, as well as incontinence, were still present in 47.7% of patients.
Although defecation dysfunction improved dramatically after surgery, 41.8 percent of patients still experienced issues 63 days later. 53.3% of patients had sexual dysfunction, and 56.6% had saddle anesthesia.
Sciatica affected 47.5% of the patients. The neurological state upon presentation and the degree of impairment are the strongest indicators of prognosis. Incomplete injuries have a better prognosis.
Diagnosing of Saddle Anesthesia
A full history is required, including inquiries about recent or past falls, trauma or injuries, anticoagulant usage, reported spine instrumentation, IV drug use, history of malignancies, chiropractic manipulations, and constitutional symptoms such as fevers/chills.
Patients may exhibit the following symptoms:
- Back pains and sciatica (as experienced in up to 97% of patients)
- Lower extremity weakness and alterations in feeling
- Bladder dysfunction (in up to 92% of cases, interruption of autonomic fibers leads to either holding or incontinence).
- Bowel dysfunction: In up to 72% of patients, bowel dysfunction causes retention or incontinence.
- Saddle anesthesia or diminished perineum feeling (in up to 93% of cases)
- Sexual impotence (impotence in men)
When presented alone, the symptoms listed above are not definite nor sensitive for conus medullaris syndrome or cauda equina syndrome. However, some of the above-mentioned signs and symptoms, when combined, should cause clinical concern.
These symptoms also have a low positive predictive value for the disorders, particularly early on. The beginning of perineal anesthesia combined with bladder dysfunction, on the other hand, is indicative of the initiation of CES and the period when the clock begins on diagnosis and care.
It is also worth noting that although painless urine retention has the highest predictive value as a standalone symptom, it is regrettably symptomatic of late, sometimes irreversible cauda equina syndrome or conus medullaris syndrome.
A comprehensive neurological examination is essential if clinical suspicion is formed based on history. Watch out for the following findings:
- Leg motor or sensory impairments: This is generally bilateral but may be unilateral or asymmetric (particularly in situations with an incomplete injury)
- Lower motor neuron symptoms in the legs: This includes areflexia, hypotonia, and atrophy (in situations of chronic cord compression which leads to cauda equina syndrome)
- Saddle anesthesia
- The rectal tone is absent or reduced.
- The bulbocavernosus reflex may be absent or diminished.
- Urinary retention is indicated by a palpable bladder.
It is crucial to highlight that impairments in the lower extremities are more typically bilateral and symmetric in isolated conus medullaris syndrome. Upper motor neuron symptoms, such as spasticity as well as hyperreflexia, may also be present.
Testing for the Saddle Anesthesia
Obtaining timely MRI imaging with sagittal as well as axial T1 and T2 sequences is the gold standard way of assessment for conus medullaris syndrome or cauda equina syndrome.
There is no set limit for "door to MRI time" in the emergency unit, although early MRI or neurosurgery, or orthopaedical consultation is critical. One hour after the patient's presentation is an excellent time frame for MRI.
A computed tomography myelogram is an alternative for individuals who are not candidates for MRI, such as people who have metal implants. Because it involves injecting contrast via a spinal tap to see the spine and its accompanying components, this imaging method has limited applicability.
To rule out urinary retention, a bladder scan should be performed to look for post-void residual volume.
Treating Saddle Anesthesia
In situations of conus medullaris and cauda equina syndromes, immediate neurosurgical or orthopedic consultation is required since the therapy is surgical decompression with laminectomy with or without following discectomy, or via sequestrectomy.
The time of decompression is debatable, with outcomes differing between instant, early, as well as late surgical decompression. Other medicinal treatments may be beneficial in certain people, based on the underlying etiology of cauda equina syndrome.
Anti-inflammatory drugs and steroids may help people with inflammatory conditions like ankylosing spondylitis. Patients experiencing cauda equina syndrome caused by an infection should be treated with antibiotics. Chemotherapy and radiation treatment should be considered for patients with spinal neoplasms.
Methylprednisolone should be given. Treatment must begin around 8 hours after the injury. There is no evidence that it is beneficial if it begins well over eight hours after injury; on the contrary, late therapy may be harmful.
Ganglioside GM1 sodium salt administration commencing within 72 hours after damage may be advantageous; the dosage is 100 mg IV once a day for 18-32 days.
Tirilazad mesylate (non-glucocorticoid 21-aminosteroid) has been found to help animals and is presently being researched. It, like glucocorticoids, suppresses lipid peroxidation and hydrolysis. All kinds of medical therapy for cauda equina syndrome should be approached with caution.
Any patient with real cauda equina syndrome who has signs of saddle anesthesia or bilateral lower limb paralysis or loss of bladder or bowel control should be seen within 24 hours. If symptoms do not improve within this time, rapid surgical decompression is required to reduce the risk of lasting brain impairment.
Decompression surgery
Acute compaction of the cauda equina or conus medullaris necessitates surgical decompression as soon as feasible. The objective is to remove the compressive agent and increase the area inside the spinal canal to alleviate pressure on the cauda equina nerves.
Cauda equina syndrome has traditionally been considered a medical emergency, requiring surgical decompression within 48 hours of the beginning of symptoms, and ideally within 6 hours after damage.
If a herniated disk is the etiology of the cauda equina syndrome, a laminectomy or laminotomy is advised to allow for canal decompression, followed by mild retraction and discectomy.
Decompression might be undertaken in a more chronic manifestation with far less severe symptoms when medically viable and should be postponed to maximize the patient's medical state; with this care, decompressing is less likely to result in lasting brain damage.
Surgical therapy for tumor removal or decompression may be required, particularly if the patient comes with an initial onset of symptoms.
Laminectomy and instrumentation or fusion for stability, as well as discectomy, are surgical options. Other surgical procedures may include wound care (for example, debridement, skin grafting, and cutaneous flap/myocutaneous flap).
Many experimental and clinical studies have reported data on functional outcomes dependent on surgical decompression time. Several studies have shown no significant variations in the level of functional improvement as a result of surgical decompression timing.
Despite these results, most researchers urge surgery by decompression as shortly as possible following the beginning of symptoms to maximize the chances of full neurologic recovery.
Patients are often moved from the surgical unit to an intensive rehabilitation facility, from where they may be released, transported to a subacute ward, or moved to long-term care, depending on their degree of long-term impairment.
Rehabilitation

As soon as feasible, the rehabilitation team, particularly the injured spinal cord rehabilitation specialist and physical and occupational therapists, should be included. In the rehabilitation unit, the team will develop targets for maintaining and increasing endurance, with the capacity to be independent in daily living activities upon release from the hospital or long-term care institution.
The aims of rehabilitation are to optimize the patient's psychological, physical, vocational, educational, medical, and social functions. To optimize medical function, provide proper treatment and prevention of the previously stated potential medical issues, including deep venous thrombosis, bowel and bladder difficulties, and decubitus ulcers.
Rehabilitation treatment

As tolerated, do a variety of movement and strengthening exercises, seated balance, transfer exercise, and tilt table (because of propensity to orthostatic hypotension). The tilt table should begin at 15 ° and gradually increase by 10 ° every 15 minutes until it reaches around 80 ° with the required safeguards.
Among the other activities are the following:
- Training in wheelchair propulsion
- Exercising on a standing table
- Increased muscular tone with functional electrical stimulation
- Extremity (lower) orthoses to help with walking and balance
- Ambulation drills
- Family education and community service
- A home exercise routine
- Occupational therapy (OT)
- Also make sure to carry out the following actions:
- Wheelchair instruction, particularly for sophisticated wheelchair activities
- Activities of daily living (ADL) training using assistance devices for clothing, grooming, eating, toileting, and bathing
- Training for motor coordination skills
- Shower schedule
- Upper extremity strength training to prepare for the increasing demands of wheelchair propulsion and assistive device walking
- Home inspection
- Family education
- A home exercise routine
For effective home ambulation and, if feasible, community ambulation, orthotic or assistive devices may be required. This includes the prescription and instruction in the right use of AFOs (ankle-foot orthoses) with canes or crutches, knee-ankle-foot orthoses (KAFO) with forearm crutches for support; for lower lesions, knee-ankle-foot orthoses (KAFOs) may be required.
In addition to the items listed above, bathtub benches, transfer boards, pressure-relieving seats, and wheelchairs may be required. Prior to release from the acute rehabilitation environment, the patient's requirements should be reviewed.
Long-term surveillance
Maintain contact with the rehabilitation team, which includes the injured spinal cord rehabilitation specialist, physical therapist, as well as occupational therapist.
These specialists are in charge of monitoring the patient's community and home integration as well as tracking gains in transfer, coordination, ambulation, strength, and activities of daily living.
Monitor post-hospital medicines and other laboratory testing with a primary care provider. Patients with either renal or bladder issues and impotence should receive frequent follow-up since they have a greater risk for recurrent urinary tract infections including calculi.
Patients using suprapubic catheters should get a cystoscopy once a year to assist identify early bladder cancer. Urodynamic tests, renal ultrasonography, and overall cancer exams should be conducted on a regular basis.
Treatment of the Complications Caused by saddle anesthesia and How to Prevent Saddle Anesthesia
As prophylaxis for deep vein thrombosis or pulmonary embolism, people to be treated should wear anti-embolic compression socks and take subcutaneous heparin for three months.
Prophylactic use of low-molecular-weight heparin is also permitted. Ultrasonography of the lower limbs may be required as a preliminary screening test, with further follow-up. Patients with neurogenic bladder may need bladder catheterization.
The US Food and Drug Administration authorized onabotulinumtoxin A in August 2011 for urine leakage in individuals with neurologic disorders (eg, spinal injury and multiple sclerosis) who have an overactive bladder.
The treatment includes 30 intradetrusor injections administered by cystoscopy. At 12 weeks, participants who got onabotulinumtoxin A exhibited a substantial decrease in urine incontinence episodes and better urodynamics when compared to placebo.
Pressure ulcers may be avoided by removing pressure, improving the wound-healing environment, and, if required, debriding. Utilization of a phosphodiesterase type 5 inhibitor (e.g., sildenafil [Viagra]) to treat impotence is becoming more common.
Alprostadil, yohimbine, and papaverine are some more erectile dysfunction medications. An implantable penile prosthesis or vibrator stimulation might possibly be employed to stimulate coitus and/or ejaculation.
For fecal incontinence, patients may need to utilize a stool softener or do a manual evacuation.
A triple-phase bone scan may demonstrate heterotopic ossification, which is linked with an increase in blood concentrations of alkaline phosphate and phosphatase, particularly in the early stages. Stretches, disodium etidronate (twenty mg/kg once a day for 2 weeks, then 10 mg/kg for up to 12wks), radiation, and surgery by excision are all part of the treatment.
Only after the heterotopic ossification has developed or stabilized, as shown by a stabilized plain x-ray, healthy alkaline phosphatase levels, and a drop in triple-phase skeletal scan activity, is surgery performed.
Pain should be addressed according to its cause; opioids may be used in the acute situation and tricyclic antidepressants subsequently. Patients may also benefit from learning, biofeedback, and relaxation treatments.
The discomfort and diminished motor strength linked with cauda equina syndrome are caused in part by nerve root ischemia. As a consequence, vasodilatory therapy may be beneficial in certain individuals.
To pump more blood to the spinal column and nerve roots, the mean arterial pressure of blood should be kept above 90 mm Hg. Therapy with lipoprostaglandin E1 as well as its derivatives has been shown to increase blood flow towards the cauda equina area while decreasing pain and motor weakening symptoms.
This therapeutic approach should only be used for people who have mild spinal stenosis and neurogenic claudication. There was no improvement seen in individuals suffering from more serious symptoms or radicular symptoms.
To avoid contractures, orthoses should be worn. Antispasticity drugs are also recommended. Clonidine, diazepam, tizanidine, and dantrolene are some more medicines. Nerve blocks might potentially be used to treat spasticity; suitable drugs include botulinum toxin, local anesthetics, or phenol.
Healthsoothe’s Conclusion on Saddle Anesthesia
Various studies have examined prognosis and results dependent on surgical decompression time. Early surgical decompression in individuals with conus medullaris and cauda equina syndromes is linked with a better prognosis, especially when surgery is performed within 48 hours after the first presentation.
The further the compression lasts, the worse the irreversible structural and functional damage will be, and the prognosis will be.
It is crucial to highlight that the existence of bladder dysfunction before surgery has been associated with worse results regardless of decompression timing, yet timely decompression is still recommended for a better prognosis regardless of clinical condition at first presentation.
Feel free to contact us at contact@healthsoothe.com if you have further questions to ask or if there’s anything you want to contribute or correct to this article.
You can always check our FAQs section below to know more about anesthesia.
And always remember that Healthsoothe is one of the best health sites out there that genuinely cares for you.
Frequently Asked Questions about Saddle Anesthesia
How Does Cauda Equina Start?
Cauda equina syndrome can present in 2 ways: acute onset, where the symptoms and signs occur rapidly, and insidious onset, where the condition begins as lower back pain and slowly progresses to bowel and urinary incontinence. Cauda equina syndrome is most commonly caused by compression from a lumbar herniated disc.
What are the Odds of Getting Cauda Equina?
Cauda equina syndrome is a relatively rare condition, comprising around 2–6% of lumbar disc operations [16, 17, 31], with an incidence in the population thought to be between 1 in 33,000 to 1 in 100,000.
Do You Always Need Surgery for Cauda Equina?
Although leg pain is common and usually goes away without surgery, cauda equina syndrome, a rare disorder affecting the bundle of nerve roots (cauda equina) at the lower (lumbar) end of the spinal cord, is a surgical emergency.
What Does Cauda Equina Back Pain Feel Like?
Compression of the cauda equina may lead to sciatic nerve pain felt on both sides of the body, and may be experienced as a sharp, hot pain felt down the backs of the thighs and possibly into the lower legs and feet.
Can People with Cauda Equina Syndrome Walk?
Cauda equina syndrome is a medical emergency that calls for urgent surgical intervention. If patients with cauda equina syndrome do not receive treatment quickly, adverse results can include paralysis, impaired bladder, and/or bowel control, difficulty walking, and/or other neurological and physical problems.
Is Cauda Equina Surgery Safe Out of Hours?
Cauda equina syndrome (CES) can have devastating neurological sequelae if surgical treatment is delayed. However, out-of-hours surgery (weekdays from 6:00 pm to 8:00 am and all weekend operations) can potentially result in higher rates of intraoperative complications, resulting in worse outcomes.
Can You Fully Recover from Cauda Equina?
Although cauda equina syndrome is not a fatal condition, it can cause severe neurological damage. If the condition is not treated quickly enough, this damage may be irreversible, meaning a patient will not make a full recovery.
How Long After a Spinal Block Can You Walk?
At 60 min after onset of spinal anesthesia, 22 patients (100%) had recovered sensory and gross motor function, but only 36% could stand, and 8% could walk without assistance (P < 0.01). At 150-180 min after onset, 96-100% of patients achieved the levels of functional balance that permitted adequate ambulation.
Where is Saddle Anesthesia Given?
Saddle block anesthesia is a kind of low spinal block that manifests anesthesia over the saddle area, i.e., perineum, perianal area, medial aspect of legs, and thigh. A variety of agents can be introduced into the spinal canal using this procedure.
Is Saddle Block the Same as Epidural?
The main difference between spinal block and epidural is that spinal block is a single-shot, short-acting regional anesthesia injected into the spinal canal that provides anesthesia for a particular surgical procedure while epidural is a continuous, long-acting regional anesthesia injected into the space around the spinal cord.
Is Saddle Block Anesthesia Painful?
The medicine may cause nausea after your surgery. It may also cause a seizure or heart attack. Saddle block or caudal anesthesia may cause nerve damage. This may lead to long-lasting numbness or pain.
What is the Most Common Cause of Cauda Equina Syndrome?
Cauda equina syndrome is most commonly caused by a massive disc herniation in the lumbar spine (low back). A disc herniation occurs when the jelly-like core of a disc herniates, or shifts out of position, putting pressure on nearby nerves in the spine.
How Quickly Does Cauda Equina Progress?
Unlike most back problems that are longstanding or chronic, cauda equina is an acute event, like a stroke or heart attack. It most often develops rapidly, within as few as 6 to 10 hours.
How Long is Recovery After Cauda Equina Surgery?
How Long Does Saddle Block Anesthesia Last?
Between 2.5–5 mg of hyperbaric anesthetic was injected intrathecally in the sitting position and the patient remained upright for 3–10 minutes. This technique of saddle block anesthesia provides analgesia for approximately 1–3 hours.
How Do You Give a Saddle Anesthesia?
Saddle block is a spinal anesthetic restricted to the perineal area, or that part of the body in touch with a saddle. It is achieved by using a small dose of hyperbaric solution of local anesthetic and maintaining the patient in a seated position after injection. One of the major advantages is avoiding hypotension.
What Can Cause Saddle Anesthesia?
The principal causes of this syndrome are tumors, lumbar spinal stenosis, ruptured lumbar disc, arachnoiditis, and spinal fracture.
What is Saddle Anesthesia Block?
Additional resources and citations
- 1wikipedia Pudendal_anesthesia
- 2"Cauda Equina Syndrome". Retrieved 2022-10-02.
- 3Gerald L Burke, MD. "Backache from Occiput to Coccyx". Retrieved 2022-10-02.